Got COVID? Want to learn how to prepare for COVID surges and reduce your risk of Long COVID? Click here
Headaches are one of the most common non-respiratory symptoms associated with SARS-CoV-2 and COVID-19. In fact, for most, a headache was the first initial symptom of the infection. For many, the headaches resolve after recovery from the acute infection. However, headaches are also one of the most common symptoms experienced by those with Long COVID. These migraine-like headaches can often last for weeks or even months, leaving many unable to perform routine daily activities.
Headaches Are a Main Symptom of Acute COVID
While originally considered a respiratory virus, respiratory symptoms are not always the first indicator of a COVID infection. For example, for many, the first symptom is the loss of taste and/or smell (anosmia). Researchers believe that this may occur due to the virus entering the nasal cavity and crossing over into the brain. In this same way, many people often experience a severe headache in addition to the anosmia. These symptoms occur before the arrival of any respiratory symptoms, such as a cough or fever. Researchers believe that the cause of the headache is similar to that seen with anosmia.
How is a COVID Headache Different?
Many describe a COVID headache as crushing pain spread throughout the skull that can cause a pulsing or pressing pain. This pain typically worsens with physical activity or movement of the head. For this reason, many often refer to it as a migraine. However, a migraine is considered a primary headache. A COVID headache, on the other hand, is considered a secondary headache due to an underlying condition. In this case, the underlying condition is the SARS-CoV-2 viral infection. While both types of headaches produce moderate to severe pain intensity, there are some differences between a traditional migraine and a COVID headache. These can include:
- Missing common additional symptoms –
Migraines often come with nausea, vomiting, and a sensitivity to light and sound. In addition, many often experience an aura before headache onset. None of these symptoms typically accompany a COVID headache. - Different pain –
In many cases, migraines occur unilaterally, or on one side. COVID headaches are typically bilateral and affect the entire head. - Do not respond to medication –
If you have a history of migraines and take prescribed medication, you may find the COVID headache does not respond. In fact, a COVID headache is unlikely to respond to traditional headache medications in general, including over-the-counter pain medications such as acetaminophen or ibuprofen.
Headaches Continue with Long COVID
Lingering headaches are not uncommon after viral infections, so it was no surprise to see headaches become a symptom associated with Long COVID. However, the persistence and severity of headaches with Long COVID has been different than with previous viral infections. While many of these headaches do improve on their own over time, many people continue to struggle with severe headaches that can last for weeks or months. In many cases, people will have a baseline headache that gets worse from time to time, along with other Long COVID symptoms. These headaches do not respond to traditional treatment options, such as OTC pain relievers or migraine medications. For those with a previous history of headaches or migraines, they may see an increase in headache occurrences after COVID as well.
What Is Causing COVID Headaches?
Currently, the exact cause of these COVID headaches is unknown. However, researchers and clinicians have some theories.
Activation of the Trigeminovascular System
Activation of the trigeminovascular system is connected to many different chronic headache conditions, such as migraines and cluster headaches. With COVID, researchers propose that the trigeminal nerve endings in the nasal cavity may sustain direct viral damage that activates the trigeminovascular system, resulting in headaches, as well as other cognitive symptoms.
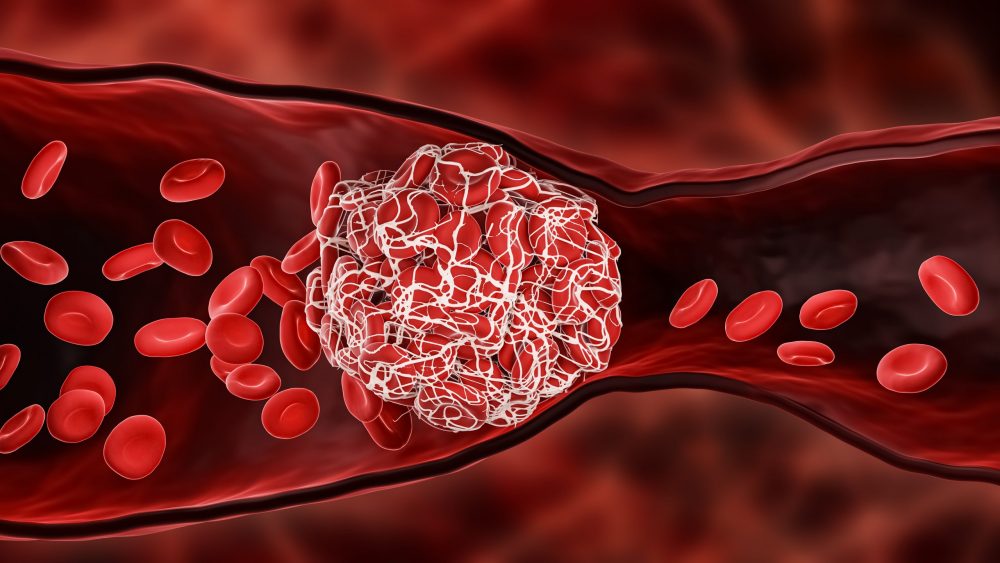
Lack of Oxygen Due to Clots
Studies are showing that many COVID patients are experiencing unusual microclots in their blood after recovering from the acute infection. These microclots can prevent adequate oxygen transportation throughout the body and contribute to Long COVID symptoms, including headaches. Research is looking into possible treatment options for these clots including anticoagulation and antiplatelet therapy. RTHM is excited to launch an anticoagulation study to improve microcirculation in Long COVID, with the hopes of reducing many Long COVID symptoms, including these severe headaches.
Damage to the Brain
Neurological damage has been seen in many COVID and Long COVID patients, but the exact cause of this damage is still unknown. Some theories believe that the virus may be able to cause direct damage to the brain by entering through the olfactory bulb or through the bloodstream or nerve endings. In addition, as your body fights the virus, your immune system often goes into overdrive, creating autoantibodies that attack healthy cells within the body and cause damage.
The Headache May Not Be in Your Head
If your headache pain focuses more around your ears and jawline, chances are you are not experiencing a headache at all, but rather jaw or dental concerns. Heavy mouth breathing during the acute COVID infection can place excess pressure on your jaw, causing the temporomandibular joint to become misaligned. This misalignment can cause headache pain in the jaw and ear area. In addition, the stress of the pandemic has increased the occurrence of teeth grinding during sleep. This grinding can contribute to headaches, as well as damage to your teeth. If your headache seems more focused in the jaw area, you may want to see your dentist to evaluate for grinding or TMJ disorders. Wearing an oral appliance can help reduce damage and pressure from grinding as well as allow your jaw to realign and heal, reducing your headache.

Get updates
Join our mailing list