Now live! RTHM Direct – simplified medication access for Long COVID, ME/CFS and related conditions. Check it out
Can you imagine getting dizzy and feeling like your heart is pounding out of your chest every time you stand up? Unfortunately, for many people with postural orthostatic tachycardia syndrome (POTS), this is exactly how they live every day! POTS is a form of dysautonomia, meaning there is a malfunction with the autonomic nervous system (ANS). This form of dysautonomia affects 1-3 million Americans and more than 10 million worldwide.
What is Postural Orthostatic Tachycardia Syndrome (POTS)?
Postural orthostatic tachycardia syndrome (POTS) is a form of orthostatic intolerance. This means the autonomic system fails to respond appropriately when a person is in an upright position. A closer look at the name explains the condition. “Postural” is related to your body’s position. “Orthostatic” refers to the position of standing upright. “Tachycardia” means an increased heart rate and “Syndrome” relates to a group of symptoms.
With POTS, people experience an exaggerated increase in their heart rate upon standing. This occurs for a variety of different reasons including lower blood volume in circulation, excessive blood pooling below the heart when the body stands upright. Sometimes this results in elevated levels of certain neurotransmitters, such as epinephrine and norepinephrine. This makes the blood vessels narrow allowing more blood to get where it needs to go, like the heart and the brain – but can lead to additional symptoms as well.
Different Types of POTS
Not all cases of POTS are the same and the cause of the autonomic dysfunction can differ from patient to patient. Understanding what contributes to a patient’s POTS can help you and your doctor choose the right treatment. The four different POTS classifications include:
- Neuropathic POTS – This form of POTS occurs due to damage to the nerves that control widening or narrowing of the blood vessels within the legs and abdomen.
- Hyperadrenergic POTS – When a person stands up, the body releases elevated levels of norepinephrine, the stress hormone, to narrow blood vessels to ensure the blood gets where it needs to go.
- Hypovolemic POTS – This form of POTS occurs due to abnormally low levels of blood in the body.
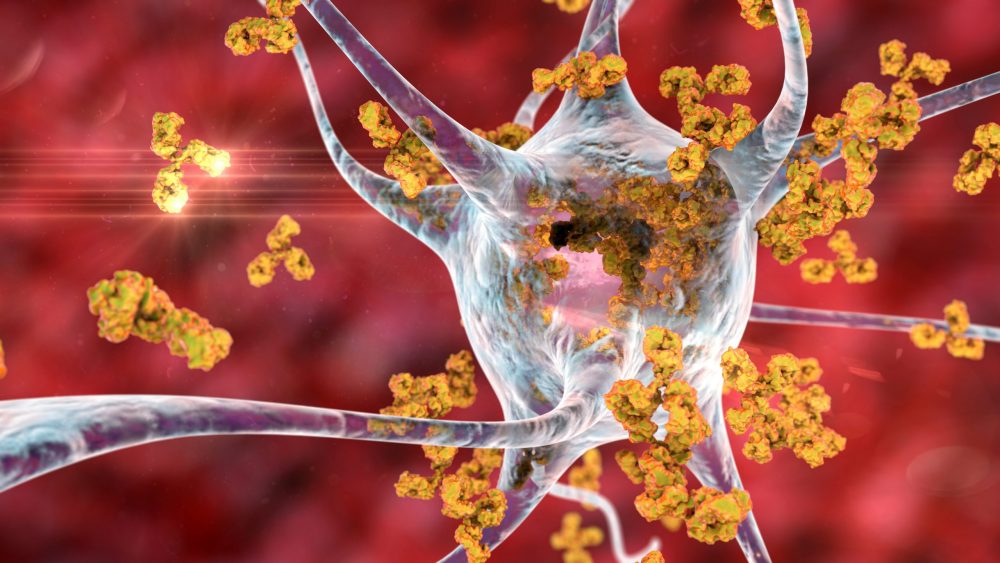
- Secondary POTS – In this case, POTS is associated with an underlying condition that causes the autonomic dysfunction, such as diabetes, Lyme disease, or autoimmune conditions, such as Sjogren’s. Some POTS is linked to the presence of autoantibodies, or immune chemicals that we produce that can attack our own tissues.
Symptoms of Postural Orthostatic Tachycardia Syndrome
When a person with POTS stands up and their heart rate jumps, they can experience a feeling of their heart pounding or racing in their chest, and they may feel dizzy. Additional symptoms can include:
- Fatigue
- Headaches
- Lightheadedness
- Heart palpitations
- Exercise intolerance
- Nausea
- Brain fog
- Fainting
- Cold and/or painful extremities
- Chest pain
- Shortness of breath
- Livid or blotchy legs
- Bulging veins in hands or feet
- Poor Blood Circulation
- Numbness
- Irritable Bowel Syndrome
- Blurred vision
Diagnostic Criteria for POTS
Diagnostic testing for POTS typically involves the use of a Tilt Table Test (TTT). This test measures changes in heart rate and blood pressure as a person is tilted from the supine (lying down) position to that of standing. Criteria for a POTS diagnosis include a heart rate increase of 30 beats per minute or more from lying down to standing, or a heart rate over 120 bpm, within the first 10 minutes of an upright tilt in adults. During this test, the blood pressure remains within normal limits. If there is a decrease in blood pressure, it is considered orthostatic hypotension while an increase in blood pressure shows orthostatic hypertension.
Other tests often used in diagnosis include the Quantitative Sudomotor Axon Reflex Test (QSART), Thermoregulatory Sweat Test, gastric motility studies, and skin biopsies that look at the small fiber nerves. Sometimes reactions may be delayed, which may indicate another autonomic syndrome such as delayed postural hypotension.
Treatment of Postural Orthostatic Tachycardia Syndrome
There is no cure for POTS, though different treatments can reduce symptoms and help improve quality of life. Treatments vary from patient to patient, but can include the following:
- Increased fluid intake – Increased water intake helps increase the fluid in your body and reduces dizziness.
- Increased salt intake – Increasing salt in the diet can help lower norepinephrine levels and reduce symptoms.
- Compression socks or tights – Wearing compression garments on the lower extremities, such as socks or tights, improves blood return to the heart and helps to reduce symptoms.
- Raising the head of your bed – This does not just mean extra pillows, but rather lifting your mattress so your entire upper body is reclined. This helps to conserve blood volume.
- Reclined exercises – Physical deconditioning (lack of movement or exercise) can worsen symptoms of POTS; however, exercise is often difficult due to dizziness and increased heart rate when standing. Reclined exercises, such as recumbent bicycling, rowing, swimming, and yoga, offer a beneficial alternative, provided the patient does not experience post-exertional malaise, the cardinal symptom of ME/CFS.
- Healthy diet – Avoiding triggers, like caffeine and high sugary foods can also reduce symptoms. A balanced diet that includes fiber, complex carbohydrates, protein, vegetables, dairy, and fruit is beneficial.
- Medications – Some medications, such as beta-blockers, SSRIs, SNRIs, salt tablets, fludrocortisone, pyridostigmine, midodrine, and others can help improve symptoms.
- Treating primary condition – In cases where POTS is secondary to another condition, improvement of the primary condition through treatment can often improve POTS symptoms.
Common POTS Comorbidities
While primary, or idiopathic, postural orthostatic tachycardia syndrome does occur, we commonly see POTS with a variety of comorbidities. Whether they contribute to the symptoms of POTS or are simply associated with the condition is often unknown. Commonly seen conditions include:
- Autoimmune diseases – Sjogren’s, lupus, sarcoidosis, and others
- Chiari malformation
- Diabetes
- Ehlers Danlos Syndrome
- Infection – Mononucleosis, Epstein Barr, Lyme, Hepatitis C, and COVID
- Multiple sclerosis
- Mitochondrial disease
- Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)
- Toxicity – chemotherapy, heavy metal poisoning, alcoholism
- Vaccinations – can trigger POTS
- Vitamin deficiencies, such as vitamin D and iron
Postural Orthostatic Tachycardia Syndrome and Long COVID
As we show above, POTS is often triggered by an infection and it seems to be a very common comorbidity found in patients with Long COVID. Unfortunately, not all physicians understand POTS and what to look for, making diagnosis often difficult. However, after a patient survey of 3,762 Long COVID patients, researchers concluded that all Long COVID patients experiencing dizziness, increased heart rate when standing, or chronic fatigue need testing for POTS and this is helping create awareness of POTS. In response to this influx of POTS patients, the American Autonomic Society issued a statement that says, “Addressing the patient needs of Long-COVID, and especially Long-COVID POTS, will take a significant investment of resources and funding, both for clinical care and research. It is imperative to act during this window of opportunity in hopes of reducing or shortening the burden of symptoms for these patients.”

Get updates
Join our mailing list