Now live! RTHM Direct – simplified medication access for Long COVID, ME/CFS and related conditions. Check it out
Long COVID, also known as post-acute sequelae of SARS-CoV-2 infection (PASC), refers to a condition in which individuals experience persistent symptoms or new symptoms that develop after the acute phase of COVID-19. While the exact mechanisms of Long COVID are not yet fully understood, viral persistence is one of the proposed explanations for this condition and one that is the subject of many research studies. To better understand the idea of viral persistence, we take a closer look at viruses and how they can act within the body.
What Is a Virus?
A virus is a microscopic infectious agent that replicates inside the cells of living organisms. It is composed of genetic material, which can be either DNA or RNA, surrounded by a protein coat called a capsid. Some viruses also have an outer envelope of lipids acquired from their host cells.
Viruses are considered intracellular parasites because they cannot reproduce or carry out metabolic processes independently. They rely on the cellular machinery of their host organisms to replicate and spread. When a virus infects a host cell, it injects its genetic material into the cell, hijacking the cellular machinery to produce more viral components. These components then assemble to form new viruses, which can infect other cells or be transmitted to new hosts.
Understanding the Different Patterns of Viral Infection
Different patterns of viral infection can be categorized into several types based on their characteristics and effects on the host. Here are the descriptions of the four common patterns: acute infection, latent infection, persistent asymptomatic infection, and persistent pathogenic infection.
Acute
Acute viral infections are characterized by a rapid onset of symptoms and a relatively short duration. The virus actively replicates within the host’s cells, leading to an immune response and the manifestation of clinical symptoms. Examples of acute viral infections include the common cold, influenza, acute gastroenteritis, and acute COVID-19.
Latent
Latent viral infections involve a period of viral dormancy or inactivity within the host’s cells. During this latent phase, the virus is not actively replicating or causing significant symptoms. However, the viral genome persists within infected cells, and under certain conditions, such as immunosuppression or other triggers, the virus can reactivate and enter an active replication phase. Herpesviruses, including herpes simplex virus (HSV) and varicella-zoster virus (VZV), are well-known examples of viruses that establish latent infections. In the case of varicella-zoster, the initial infection causes chickenpox before entering the latent stage. When reactivated, the patient experiences shingles.
Persistent – Asymptomatic
In this type of viral infection, the virus persists within the host for an extended period without causing noticeable symptoms. The infected individual may remain asymptomatic throughout the infection, but they can still transmit the virus to others. Hepatitis B virus (HBV) and hepatitis C virus (HCV) are examples of viruses that can cause persistent asymptomatic infections, although in some cases, they can become pathogenic over time.
Persistent – Pathogenic
Persistent pathogenic infections are characterized by ongoing viral replication and the presence of clinical symptoms or disease progression. The virus actively persists within the host and continues to cause tissue damage, inflammation, and other pathological effects. Examples include human immunodeficiency virus (HIV), which causes acquired immunodeficiency syndrome (AIDS), and hepatitis C virus (HCV), which can lead to chronic liver disease.
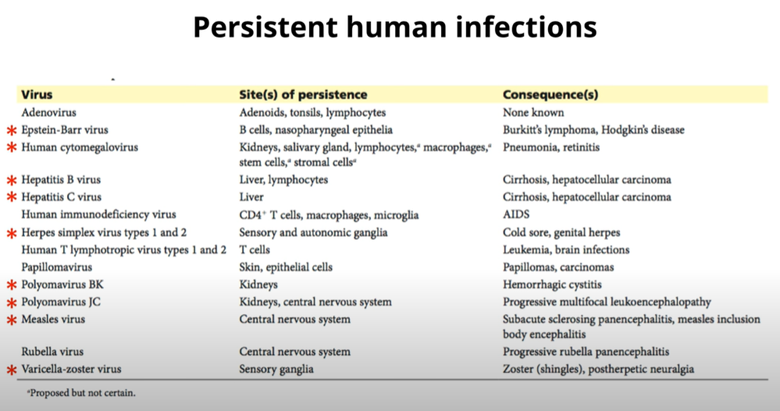
Image from Virology Lectures 2023 #17: Persistent Infections
What is Viral Persistence?
Viral persistence refers to the ability of certain viruses to establish a long-term or chronic infection within a host organism. Unlike acute viral infections, which are typically cleared by the immune system within a relatively short period of time, persistent viruses can evade immune responses and maintain a presence in the host.
Viral persistence can have various consequences. In some cases, persistent viral infections may be asymptomatic or cause mild symptoms. In contrast, in others, they can lead to chronic inflammation, tissue damage, or an increased risk of developing complex illnesses or certain cancers. Understanding the mechanisms of viral persistence is crucial for developing effective treatments and preventive measures against these persistent infections.
Difference Between Viral Persistence and Viral Reactivation
Viral persistence and viral reactivation are related concepts but have distinct meanings in the context of viral infections.
Viral persistence refers to the ability of a virus to establish and maintain a long-term or chronic infection within a host organism. In persistent infections, the virus replicates and persists in the host’s cells for an extended period, often evading or modulating the immune response. This persistence can lead to a sustained presence of the virus in the host’s body, potentially causing chronic inflammation, tissue damage, or other long-term effects.
On the other hand, viral reactivation refers to the process by which a latent or dormant virus that has been residing within the host’s cells reactivates and resumes active replication. During viral latency, the virus remains in a dormant state, with its genetic material integrated into the host cell’s genome. Reactivation can occur spontaneously or in response to various triggers, such as stress, immunosuppression, hormonal changes, or other infections, such as SARS-CoV-2. The reactivated virus then resumes its replication cycle, leading to the recurrence of symptoms or the shedding of infectious particles.
Viral Persistence in Long COVID
Viral persistence in Long COVID refers to the possibility that the SARS-CoV-2 virus may continue to replicate or remain present in certain tissues or cells of the body even after the acute infection has resolved. This persistence can contribute to ongoing symptoms and inflammation and may be the underlying mechanism behind Long COVID. However, it’s important to note that the extent and significance of viral persistence in Long COVID are still being actively studied, and research in this area is ongoing.
Several studies have suggested the presence of viral genetic material or remnants of SARS-CoV-2 in various tissues and organs, including the respiratory tract, gastrointestinal tract, cardiovascular system, and central nervous system, in some Long COVID patients. However, it remains unclear whether these viral remnants are viable and capable of replication, or if they are remnants of the initial infection that are triggering an ongoing immune response.
Recent Research Looking at Viral Persistence and Long COVID
Viral Persistence, Reactivation, and Mechanisms of Long COVID
Why Viral Reservoirs Are a Prime Suspect for Long COVID Sleuths
SARS-CoV-2 Infection and Persistence in the Human Body and Brain at Autopsy
How Long Does COVID-19 Linger in Your Body? New Report Offers Clues
Mechanistic Pathways of PASC Session 2: Viral Persistence and Viral Reservoirs
While more research is needed to establish a direct link between viral persistence and Long COVID, some scientists consider viral reservoirs to be a leading driver of this condition. The ongoing efforts to understand the pathophysiology of Long COVID can help improve diagnostic and therapeutic procedures for this often life-altering condition. Clinicians at RTHM are working tirelessly to find and identify the underlying mechanisms, including viral persistence, of Long COVID and develop effective solutions to help treat the symptoms those with Long COVID and other viral-associated conditions experience.

Get updates
Join our mailing list