Now live! RTHM Direct – simplified medication access for Long COVID, ME/CFS and related conditions. Check it out
Neuro-ophthalmologic disorders are a group of conditions that involve abnormalities in the visual system resulting from underlying neurological issues. These disorders affect the intricate relationship between the eyes, optic nerves, and the brain, leading to various visual symptoms and eye-related abnormalities. Disruptions in those intricate relationships can be the result of many underlying conditions, including Long COVID, ME/CFS, and other common comorbidities, such as connective tissue disorders like Ehlers-Danlos syndrome. Here we look closely at neuro-ophthalmologic disorders, how they can contribute to many of your symptoms, and the treatment options available.
What is Neuro-Ophthalmology?
Neuro-ophthalmology is a specialized field of medicine that focuses on the intersection of neurology and ophthalmology. It deals with the diagnosis and management of visual disturbances and eye conditions that are related to underlying neurological disorders. Neuro-ophthalmologists are medical doctors who have completed specialized training in both neurology and ophthalmology, enabling them to evaluate and treat patients with complex visual and neurological issues.
The visual system is intricately connected to the brain, and any abnormalities or diseases affecting the neurological pathways involved in vision can result in visual symptoms.
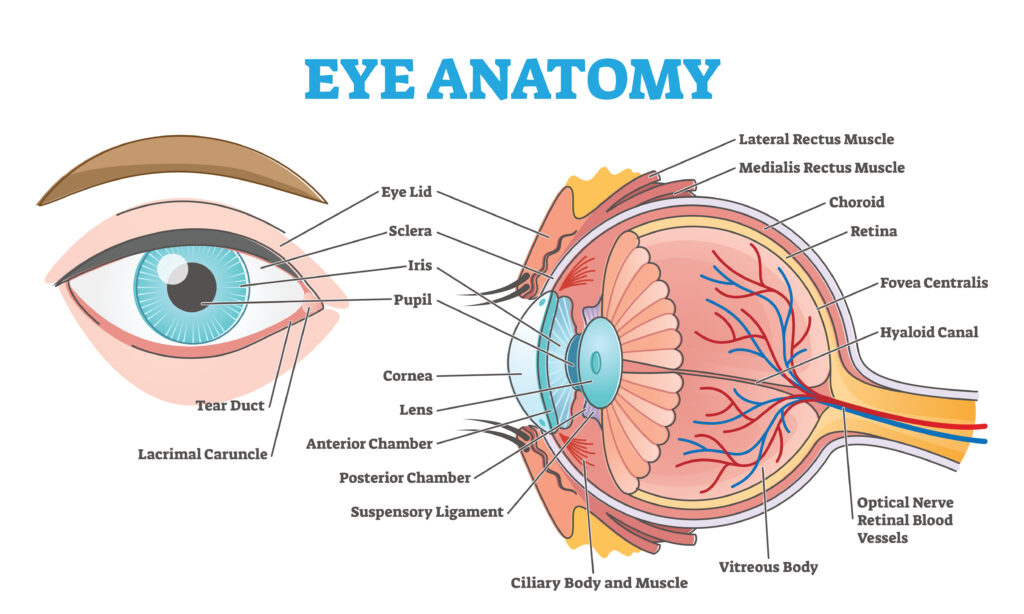
Here is a diagram of the structures within the eye, to help with some of the terms used in the list below:
Conditions commonly managed by neuro-ophthalmologists include:
-
Optic nerve disorders: These include optic neuritis (inflammation of the optic nerve), optic neuropathies (damage to the optic nerve), and compressive optic neuropathies caused by conditions like tumors or aneurysms.
-
Visual field defects: Neuro-ophthalmologists evaluate and manage various types of visual field abnormalities caused by conditions such as strokes, brain tumors, or neurodegenerative diseases.
-
Cranial nerve disorders: The cranial nerves that control eye movements (e.g., oculomotor nerve, trochlear nerve, abducens nerve) can be affected by neurological conditions, leading to eye movement abnormalities or double vision.
-
Disorders of pupillary function: Neuro-ophthalmologists assess pupillary abnormalities, such as anisocoria (unequal pupil size) or abnormal pupillary responses, which may indicate underlying neurological issues like Horner’s syndrome or Adie’s tonic pupil.
-
Visual disturbances related to systemic neurological diseases: Neuro-ophthalmologists evaluate and manage visual symptoms associated with conditions like multiple sclerosis, myasthenia gravis, stroke, or brain tumors.
-
Thyroid eye disease: This condition involves eye-related manifestations associated with autoimmune thyroid disease. Neuro-ophthalmologists play a role in managing ocular manifestations and associated visual disturbances.
-
Headaches and migraines: Neuro-ophthalmologists can assist in diagnosing and managing headaches and migraines that are accompanied by visual symptoms or ocular manifestations.
Neuro-ophthalmology requires a multidisciplinary approach, involving collaboration with other specialists such as neurologists, neurosurgeons, rheumatologists, or radiologists. By combining knowledge from both neurology and ophthalmology, neuro-ophthalmologists provide comprehensive care for patients with complex visual and neurological conditions.
Visual Symptoms Seen with These Disorders
Neuro-ophthalmologic conditions can manifest with various symptoms, which may include:
-
Visual disturbances: Patients may experience blurred vision, double vision (diplopia), or decreased visual acuity. They may also have difficulty focusing or maintaining visual fixation.
-
Optic nerve abnormalities: Conditions affecting the optic nerve, such as optic neuritis or optic neuropathy, can lead to visual symptoms such as reduced color vision, loss of peripheral vision (typically in a specific pattern, e.g., central scotoma), or visual field defects.
-
Eye movement abnormalities: Neuro-ophthalmologic disorders can cause abnormal eye movements, including involuntary eye movements (nystagmus), limited eye movements (ophthalmoplegia), or misalignment of the eyes (strabismus).
-
Pupillary abnormalities: Dysfunction in the pupillary reflexes may occur, leading to abnormalities in the size (anisocoria) or reactivity of the pupils. This can be seen in conditions like Horner’s syndrome or Adie’s tonic pupil.
-
Visual field defects: These defects can manifest as areas of reduced or absent vision in specific parts of the visual field. Depending on the location and extent of the visual pathway involvement, various patterns of visual field defects can occur.
-
Headaches: Some neuro-ophthalmologic conditions, such as migraines or certain types of optic neuritis, may present with headaches, often associated with visual symptoms.
-
Facial or eyelid abnormalities: Certain conditions affecting the nerves that control facial and eyelid movements can cause weakness or paralysis of the muscles, leading to drooping of the eyelid (ptosis) or asymmetry of facial expressions.
It’s important to note that the specific symptoms experienced can vary depending on the underlying condition and the structures involved.
Some common symptoms that may not be immediately obvious as stemming from Neuro-ophthalmological problems are as follows:
-
You may find you get nauseated watching a moving object (like a swinging pendulum).
-
You may get “car sick” or motion sickness more easily.
-
Find that you now struggle to remember or comprehend what you are reading.
-
You may notice that your eyes “jump” to the end of a line of text when you try to read, instead of scanning smoothly along the text from left to right.
-
You may notice that you have to re-read the same line of text a few times or use your finger or a highlighter to guide your eyes along the line of text in order to comprehend it.
When the eyes are not working together correctly, or with the brain correctly, even in subtle ways, the brain has to work extra hard to read, track movement, etc. possibly contributing to brain fog, headaches, fatigue, or PEM crashes from cognitive exertion. Some patients notice a significant reduction in headaches and improvement in cognitive exertional tolerance with interventions and therapies like prism lenses, vision therapy, tinted lenses, and more.
At-Home Testing and Evaluation
Before talking with your provider, there are some at-home tests and modifications you can try to see if you have elements of a visual processing disorder.
To test whether different background colors make it easier for you to read, reduce strain on your eyes, and/or improve reading comprehension, try changing the background color of this website by clicking on the colored pairs of glasses at the top of the page, and seeing if a particular background color makes it easier for you to read the text on the page.
The same site also has quizzes to see if you have Irlen Syndrome, a perceptual processing disorder where the brain has trouble processing visual information from the eyes that can be helped by using colored filters on screens, overlays for books, or colored lenses in one’s glasses.
Vision therapy helps retrain the connection between the eyes and the brain. Generally, it is not covered by insurance and requires going to a provider’s office regularly. However, here are two at-home vision therapy options recommended by Dr. Singman from Hopkins Neuro-ophthalmologist: Vizual Edge & Home Vision Therapy Solutions HTS. Both are able to be done at home, in shorter time intervals to start out (so you can get used to it first), and for a cheaper price.
Diagnosing Neuro-Ophthalmological Disorders
The diagnosis of neuro-ophthalmologic conditions involves a comprehensive evaluation that combines clinical assessment, specialized tests, and imaging studies. The following are commonly used methods for diagnosing these conditions:
-
Medical history and physical examination: The healthcare provider will take a detailed history to understand your symptoms, their duration, and any relevant medical conditions. A comprehensive physical examination will be conducted, including a thorough assessment of your vision, eye movements, pupillary reflexes, and the structure of the eye.
-
Visual acuity and visual field testing: Visual acuity measures the sharpness of your vision, typically using an eye chart. Visual field testing evaluates your peripheral vision and can help identify any areas of reduced or absent vision.
-
Ophthalmoscopy: This examination involves looking into the eye with a specialized instrument called an ophthalmoscope to assess the health of the optic nerve, retina, and blood vessels in the eye.
-
Pupillary examination: The healthcare provider will evaluate the size, shape, and reactivity of your pupils using a penlight or specialized pupillometer.
-
Eye movement evaluation: Various tests can assess eye movements and coordination, such as the assessment of smooth pursuit, saccades, and nystagmus.
-
Neurological examination: A thorough neurological examination may be performed to evaluate other neurological signs or symptoms that could be associated with the condition. This may include assessing muscle strength, reflexes, coordination, and sensation.
-
Ancillary testing: Additional tests may be ordered based on the suspected condition. These can include neuroimaging studies such as magnetic resonance imaging (MRI) or computed tomography (CT) scans to assess the brain, optic nerves, or other structures. Other specialized tests may include electroretinography (ERG), electrooculography (EOG), visual evoked potentials (VEP), or blood tests for specific markers.
The specific diagnostic approach will depend on the suspected condition and the individual patient’s needs. A neuro-ophthalmologist is typically involved in the evaluation and diagnosis process and will coordinate care with your primary clinician.
Good videos detailing neuro-ophthalmology exams:
The Neuro-ophthalmology Exam: Neuro
The Neuro-ophthalmology Exam: Pupils; Color; Eye Movements; Prism
The Neuro-Ophthalmology Exam Playlist.
Treating Neuro-Ophthalmological Diseases
The treatment for neuro-ophthalmological diseases depends on the specific condition and its underlying cause. Since neuro-ophthalmological disorders involve abnormalities in both the visual system and the nervous system, the management often requires a multidisciplinary approach involving neuro-ophthalmologists, neurologists, ophthalmologists, neurosurgeons, and other specialists. The specific treatment plan for a neuro-ophthalmological disease should be tailored to the individual patient’s needs and goals. Here are some general treatment approaches used for neuro-ophthalmological diseases:
-
Medications: Pharmacological treatment may be employed to address the underlying cause or manage specific symptoms associated with the condition. For example, anti-inflammatory medications or immunosuppressive drugs can be used to treat inflammatory conditions like optic neuritis or autoimmune disorders affecting the optic nerve. Medications to control pain, reduce intraocular pressure, or manage vascular conditions may also be prescribed based on the specific situation.
-
Neurosurgical interventions: In cases where neuroimaging reveals structural abnormalities or lesions that are causing the symptoms, surgical interventions may be necessary. Neurosurgeons can perform procedures to remove tumors, relieve compression on the optic nerves or other structures, or manage conditions like hydrocephalus that may impact the visual system.
-
Vision rehabilitation: For individuals with permanent vision loss or visual impairment, vision rehabilitation programs can help maximize their remaining vision and improve functional abilities. These programs may involve low vision aids, assistive technologies, training in adaptive techniques, and counseling to support adjustment and coping strategies. Here are 2 at-home vision therapy options recommended by Dr. Singman at Hopkins: Vizual Edge & Home Vision Therapy Solutions HTS
-
Symptomatic management: Some conditions may not have a specific cure, but symptomatic management can help alleviate the associated symptoms. For example, prism lenses or other corrective lenses may be prescribed to address double vision (diplopia), while medications or botulinum toxin injections can manage abnormal eye movements (nystagmus). Some people may benefit from using colored filters or lenses over reading material. You can try changing the background color of this website by clicking on the colored glasses at the top of the page, and seeing if a particular color makes it easier for you to read the text on the page.
-
Treatment of underlying systemic conditions: In cases where the neuro-ophthalmological disorder is associated with a systemic disease, such as multiple sclerosis, thyroid eye disease, or vasculitis, treating the underlying condition is a crucial component of management. This may involve systemic medications, immunosuppression, or targeted therapies specific to the underlying disease.
Neuro-Ophthalmological Disorders with Long COVID
Long COVID, also known as post-acute sequelae of SARS-CoV-2 infection (PASC), refers to persistent symptoms that can occur following a COVID-19 infection. While the focus of research on Long COVID is still evolving, there is increasing recognition of neurological and ophthalmological manifestations associated with this condition. Neuro-ophthalmological disorders may be among the various symptoms experienced by individuals with Long COVID. Some potential neuro-ophthalmological manifestations reported in Long COVID include:
-
Visual disturbances: Visual symptoms such as blurred vision, difficulty focusing, and photophobia (sensitivity to light) have been reported by some individuals with Long COVID. These symptoms may be transient or persist for an extended period.
-
Optic neuropathy: There have been reports of optic neuropathy, which refers to damage or dysfunction of the optic nerve. This can result in visual field defects, reduced visual acuity, or other visual impairments.
-
Eye movement abnormalities: Long COVID patients may experience abnormalities in eye movements, such as nystagmus (involuntary eye movements), saccadic abnormalities (problems with quick, precise eye movements), or oculomotor dysfunction.
-
Pupillary abnormalities: Some individuals have reported pupillary abnormalities, including unequal pupil size (anisocoria) or abnormal pupillary responses.
-
Dry eyes: Dry eye symptoms, such as dryness, grittiness, and discomfort in the eyes, have been reported.
-
Cranial nerve palsies: Dysfunction of cranial nerves that control eye movements (such as the oculomotor, trochlear, and abducens nerves) can occur in Long COVID, leading to double vision (diplopia) or other eye movement abnormalities.
It is important to note that the understanding of Long COVID is still developing, and research is ongoing. The exact mechanisms underlying these neuro-ophthalmological symptoms are not yet fully understood.
A review in Clinical & Experimental Ophthalmology details four possible mechanisms by which an acute COVID-19 infection can contribute to neuro-ophthalmological complications. These include:
-
Effects of severe pulmonary disease on the neural axis
-
Endothelial dysfunction
-
Dysimmune responses directed against the neuraxis
-
Direct neuroinvasion and injury from the virus
In addition, a study published in the British Journal of Ophthalmology identified a link to a loss of corneal nerve fibers as well as an increase in dendritic cells in some patients with Long COVID. This is especially true in those experiencing neurological symptoms.
If you are experiencing neuro-ophthalmological symptoms following a COVID-19 infection, it is recommended to consult with your clinician. They can evaluate your symptoms, conduct necessary tests, and provide appropriate management and support based on your individual condition.
Additional Studies on Long COVID and Neuro-ophthalmologic Complications
Neuro-ophthalmologic complications of coronavirus disease 2019
Neuro-Ophthalmological Disorders after COVID Vaccination
In addition to neuro-ophthalmologic conditions potentially caused by the SARS-CoV-2 virus, studies show a possible connection between these conditions and the COVID-19 vaccination. Studies like this one show a potential connection and recommend that “As COVID-19 vaccines can cause neuro-ophthalmological conditions, such as oculomotor nerve palsy, patients’ age, and underlying diseases should be considered before vaccine administration.”
There have also been several case reports of elevated intracranial pressure after COVID-19 vaccination. There is a case of a 15 y/o girl after the original Pfizer vaccine, a 23 y/o man after the Astra Zeneca vaccine, and another case of a young man developing high intracranial pressure after the Sputnik V vaccine. Elevations in pressure inside of the head frequently cause headaches and vision changes as well as other neuro-ophthalmological symptoms. Treatment varies but can include medications or procedures to lower pressure in the head by lowering the production of cerebrospinal fluid (CSF), draining CSF, shunting CSF to another part of the body, or increasing the absorption of CSF.
Neuro-Ophthalmological Disorders with ME/CFS
The relationship between neuro-ophthalmological disorders and myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) is an area of ongoing research and investigation. ME/CFS is a complex condition characterized by persistent fatigue, post-exertional malaise, cognitive impairments, and a range of other symptoms.
While the specific connection between neuro-ophthalmological disorders and ME/CFS is not yet fully understood, there is emerging evidence suggesting that visual symptoms and ophthalmological abnormalities may be present in a subset of individuals with ME/CFS. These symptoms can include blurred vision, sensitivity to light (photophobia), eye pain, and problems with visual accommodation and focus.
One possible explanation is that ME/CFS involves dysfunction in the autonomic nervous system, which regulates various bodily functions, including those related to vision. Autonomic dysfunction may contribute to altered blood flow regulation and abnormal neurochemical responses within the visual system.
“Neuro-ophthalmological disorders in myalgic encephalomyelitis/chronic fatigue syndrome,” published in the journal Medical Hypotheses, explore the potential association between neuro-ophthalmological disorders and myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS). This study proposes that ME/CFS may involve dysfunction in the autonomic nervous and visual systems, leading to various neuro-ophthalmological manifestations.
The study suggests that patients with ME/CFS may experience visual symptoms and ophthalmological abnormalities, such as reduced visual acuity, photophobia (sensitivity to light), accommodative dysfunction (problems with focusing), and impaired pupillary responses.
However, it’s important to note that research in this area is still limited, and more studies are needed to establish the nature and prevalence of neuro-ophthalmological disorders in ME/CFS. The relationship between these two entities remains complex and multifaceted, involving interactions between the immune system, nervous system, and other physiological processes.
If you have ME/CFS and are experiencing visual symptoms or concerns, it is important to talk with your clinician and other healthcare professionals familiar with both ME/CFS and neuro-ophthalmology. They can provide a comprehensive evaluation and appropriate management based on your individual symptoms and needs.
Additional Information on ME/CFS and Neuro-Ophthalmological Disorders
Visual Dysfunction in Chronic Fatigue Syndrome
Neuro-Ophthalmological Disorders with EDS and Other Structural and Connective Tissue Disorders
Ehlers-Danlos Syndrome
Ehlers-Danlos Syndrome (EDS) is a group of genetic connective tissue disorders that can affect multiple systems in the body, including the eyes and the nervous system.
Neuro-ophthalmological disorders can occur in individuals with EDS and may involve various visual and neurological symptoms. Some neuro-ophthalmological disorders that can be associated with EDS include:
-
Ocular manifestations: EDS can affect the structure and function of the eyes, leading to several ocular manifestations. These can include:
-
Keratoconus: This condition involves thinning and bulging of the cornea, leading to visual distortion and astigmatism.
-
High myopia: EDS may be associated with a higher risk of developing severe nearsightedness (near objects are clear, objects at a distance are out of focus)
-
Astigmatism: Irregular curvature of the cornea can cause astigmatism, resulting in blurred or distorted vision.
-
Retinal detachment: EDS can increase the risk of retinal detachment, which is a potentially sight-threatening condition. Symptoms can include the sudden onset of a lot of “floaters,” a curtain-like shadow over one’s vision, flashes of light in one or both eyes, gradually reducing one’s side (peripheral) vision, etc.
-
Strabismus and amblyopia: EDS can be associated with strabismus, which is the misalignment of the eyes, and amblyopia, commonly known as lazy eye. These conditions may require ophthalmic interventions, such as patching or corrective lenses, to improve visual function.
-
Cranial nerve palsies: EDS may increase the risk of cranial nerve palsies, affecting the nerves responsible for eye movement and visual function. This can lead to diplopia (double vision), ptosis (drooping eyelid), or other eye movement abnormalities.
Neuro-ophthalmologic disorders are common in patients with EDS and should be carefully evaluated during ophthalmologic examinations.
Dr. Singman from Johns Hopkins, gave an excellent talk about Neuro-ophthalmological symptoms and conditions in EDS that is worth a watch!
Idiopathic Intracranial Hypertension
Pseudotumor cerebri, also known as idiopathic intracranial hypertension (IIH), is a condition characterized by increased pressure within the skull (intracranial pressure) without the presence of a tumor. It primarily affects women of childbearing age, but it can occur in individuals of any age or gender. Pseudotumor cerebri can lead to various neuro-ophthalmological manifestations due to the increased pressure on the optic nerve and surrounding structures. Some of these manifestations include:
-
Headaches: Headaches are a common symptom of pseudotumor cerebri. Headaches can be severe and persistent or episodial in nature. Changes in posture or physical exertion can worsen these headaches.
-
Visual disturbances: Visual symptoms are a hallmark of pseudotumor cerebri. These may include transient visual obscurations (temporary dimming or loss of vision), blurred vision, double vision (diplopia), or vision loss. These symptoms are often related to the compression or swelling of the optic nerve and can vary in severity.
-
Papilledema: Papilledema refers to swelling of the optic nerve head, which providers detect during a comprehensive eye examination. Papilledema occurs due to increased pressure within the skull. Visual changes, such as decreased visual acuity or visual field defects, can also occur.
-
Transient visual obscurations (TVOs): TVOs are brief episodes of visual dimming or blackouts that can last for seconds to minutes. Changes in head position or activities that increase intracranial pressure can trigger these.
-
Visual field defects: Pseudotumor cerebri can cause visual field abnormalities, which are changes in peripheral or central vision. These defects can manifest as blind spots or loss of vision in specific areas of the visual field.
-
Other neuro-ophthalmological manifestations: Pseudotumor cerebri can also lead to other ocular manifestations, such as sixth nerve palsy (causing eye misalignment), pulsatile tinnitus (ringing in the ears synchronized with the heartbeat), and dizziness.
Management of pseudotumor cerebri aims to reduce intracranial pressure and prevent vision loss. Treatment options may include medications to reduce cerebrospinal fluid production or increase its absorption, and, in some cases, surgical interventions such as optic nerve sheath fenestration or cerebrospinal fluid shunting.
Chiari Malformation
Chiari malformation is a structural abnormality in which the lower part of the brain, known as the cerebellum, extends into the upper spinal canal. This can result in compression of the brainstem and disruption of the normal flow of cerebrospinal fluid (CSF). Chiari malformation is classified into different types based on the severity and extent of the malformation.
Neuro-ophthalmological manifestations can occur in individuals with Chiari malformation due to the compression and displacement of neural structures. Some of the neuro-ophthalmological symptoms associated with Chiari malformation include:
-
Headaches: Headaches, particularly at the back of the head (occipital headaches), are a common symptom of Chiari malformation. They can be severe, worsen with straining or coughing, and may be accompanied by neck pain.
-
Visual disturbances: Chiari malformation can cause various visual symptoms, including blurred or double vision, sensitivity to light (photophobia), eye movement abnormalities, and difficulty focusing. These symptoms can be a result of compression or stretching of the nerves involved in vision.
-
Papilledema: Chiari malformation can lead to increased intracranial pressure, which can cause swelling of the optic nerve head, known as papilledema. Papilledema is detected during a comprehensive eye examination and may result in visual impairment or changes in visual fields.
-
Nystagmus: Nystagmus refers to involuntary, rhythmic eye movements. It can occur as a result of disruption to the normal functioning of the brainstem and cerebellum due to Chiari malformation.
-
Cranial nerve abnormalities: Compression of the cranial nerves within the skull can occur in Chiari malformation, leading to cranial nerve abnormalities. This can cause symptoms such as ptosis (drooping eyelid), pupillary abnormalities, or weakness of eye movements.
Other associated symptoms may include neck pain, dizziness, difficulty swallowing, and numbness or weakness in the extremities.
Treatment for Chiari malformation depends on the severity of symptoms and the type of malformation. Mild cases may be managed conservatively with pain medication and symptom management, while more severe cases may require surgical intervention to decompress the brain and restore normal CSF flow.
It is important to note that the presence and severity of neuro-ophthalmological disorders in individuals with Long COVID, ME/CFS, EDS, pseudotumor cerebri, and Chiari malformation vary from patient to patient. Oftentimes, visual symptom manifestations lead to an initial diagnosis, such as in these case presentations.

Get updates
Join our mailing list