Now live! RTHM Direct – simplified medication access for Long COVID, ME/CFS and related conditions. Check it out
As the COVID pandemic began to spread across the world, we focused on avoiding the virus and surviving the infection. However, we quickly learned that the initial infection is only part of the COVID concerns that we face. For 10-30 percent of COVID patients, acute infection recovery is often short-lived, if ever achieved. Many people continue to experience COVID symptoms well past the typical 4-week mark. Others develop new symptoms weeks to months later. Known as Long COVID, this new condition causes a variety of different symptoms and concerns, including chest pain and pressure.
Disclaimer: New symptoms of chest pain and pressure should be evaluated by a medical professional immediately to rule out potential life-threatening conditions, such as a heart attack or pulmonary embolism. While chest pain and pressure are symptoms experienced by those with Long COVID, you must first rule out any life-threatening conditions.
Possible COVID-Related Heart Injury
In addition to the respiratory system, the SARS-CoV-2 virus also infects the heart and the blood vessels within the body. Three main heart complications seen with acute COVID include myocarditis, pericarditis, and heart arrhythmias. Myocarditis is the inflammation of the heart muscle while pericarditis is the inflammation of the outer heart lining. Heart arrhythmias can include tachycardia (high heart rate) or bradycardia (slow heart rate). All these conditions can contribute to chest pain and pressure. If left untreated and monitored, they can contribute to more serious concerns.
Studies find that heart damage is very common with acute COVID but even occurs in those with mild infection. An early cardiology study shows that 78% of recovered patients show heart abnormalities 2-3 months after acute infection recovery. The American Heart Association recommends you see a physician if you experience any of the following new symptoms during recovery:
- Chest pain
- Increasing shortness of breath
- Ankle swelling
- Heart arrhythmias
- Lightheadedness
- Dizziness
Hidden Lung Damage from Acute Illness
As a respiratory virus, the fact that SARS-CoV-2 contributes to lung damage was no surprise. Pneumonia is a common occurrence with severe COVID, as is acute respiratory distress syndrome (ARDS). The infection damages tissue in the lungs. In most cases, the lungs can recover. However, as the lungs heal, you can experience coughing, shortness of breath, and chest pain and pressure.
In severe, acute COVID cases, the lungs may sustain damage that will not heal. This leads to pulmonary fibrosis, or scarring of the lung tissue, also known as interstitial lung disease (ILD). This scarring does not heal and contributes to a wide variety of symptoms, including shortness of breath, shallow breathing, and a dry cough that can cause chest pain and soreness. ILD requires regular follow-up to monitor disease progression, and, in severe cases, a transplant may be necessary.
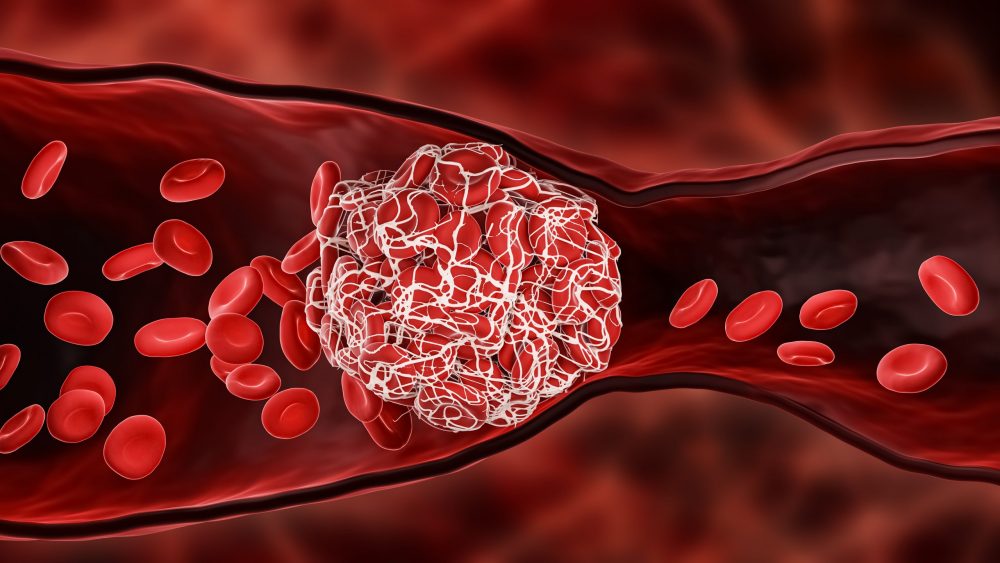
As we learn more about SARS-CoV-2 and COVID, we are seeing that it is not uncommon to cause microclots in the blood. These clots have increased the risk of pulmonary embolism in both acute COVID cases, as well as in those with mild or asymptomatic disease. In those with mild disease, thromboembolic events can occur weeks after initial infection and after acute infection recovery. Symptoms of a pulmonary embolism can include sudden shortness of breath, chest pain that gets worse with breathing, irregular heartbeat, coughing, dizziness, and lightheadedness. A pulmonary embolism is an emergency and if you suddenly experience these symptoms, it is important to seek medical attention immediately.
When Traditional Tests Miss Potential Damage
Even if routine testing shows no obvious lung damage, new research is showing that traditional testing methods may not be enough when it comes to identifying lung damage after COVID. Using hyperpolarized xenon MRI (XeMRI) scans, researchers were able to find lung abnormalities in Long COVID patients that were not detectable with routine CT scans. They discovered that this damage is limiting oxygen from entering the bloodstream as is necessary, and this limited oxygen is contributing to breathing abnormalities and other symptoms, such as chest pain or tightness.
Dysautonomia and Postural Orthostatic Tachycardia Syndrome (POTS)
If all cardiac and pulmonary tests return normal and you are still experiencing chest pain, heart arrhythmias, and symptoms such as lightheadedness and dizziness upon standing, another possible condition seen with Long COVID is postural orthostatic tachycardia syndrome or POTS. This is a condition of the autonomic nervous system (ANS) and is one of many different autonomic conditions known as Dysautonomia. The ANS regulates body functions that you do not physically control, such as breathing, heart rate, digestion, blood pressure, kidney function, and body temperature regulation. Unfortunately, SARS-CoV-2 can contribute to damage in the ANS. POTS is the most common form of dysautonomia in general, as well as the most common form we are seeing with Long COVID.
We offer in-depth information on both dysautonomias (CLICK HERE) and POTS (CLICK HERE) to help you better understand these conditions.
Endothelial Dysfunction and Microclots
In addition to the possible causes above, research shows that the SARS-CoV-2 virus targets the endothelium. The endothelium is the thin membrane lining the inside of blood vessels throughout the body. Endothelial cells help release enzymes that regulate blood clotting, platelet adhesion, vascular contraction and relaxation, and immune function. When the endothelium sustains damage, it affects the release of these enzymes. Disruption in these key functions can cause microclots in the blood. These microclots can block oxygen transportation through the body. In addition, inappropriate relaxation and contraction of blood vessels can also disrupt oxygen transport. This endothelial dysfunction can contribute to symptoms such as chest pain and shortness of breath.

Get updates
Join our mailing list