Now live! RTHM Direct – simplified medication access for Long COVID, ME/CFS and related conditions. Check it out
Mast cells are found throughout the body and play a complex and critical role in the immune response of a healthy body. However, when these cells become altered or activate inappropriately to specific triggers, they can create symptoms throughout the body. While mast cell activation syndrome (MCAS) is often misunderstood and only recently being understood and diagnosed by clinicians, the prevalence of this syndrome is widespread and, as researchers learn more, mast cell activation may play a role in many other chronic conditions, such as POTS and Long COVID.
What are Mast Cells?
Mast cells are a type of white blood cell that is found in tissue throughout the body. These specialized cells play an important role in a healthy immune system, allowing the body to fight bacterial, viral, and parasitic infections. These cells are filled with mediators of immune function, including cytokines, growth factors, histamine, and heparin. The mast cells release these chemicals in response to changes within their environment, such as allergens or an immune response. The release of these chemicals contributes to symptoms typically seen during an allergic reaction, such as flushing and itching. However, when problems arise within these cells, such as inappropriate or excessive chemical release, a person can experience more severe symptoms, such as abdominal cramping, diarrhea, nausea, muscle pain, low blood pressure, and, in severe cases, anaphylaxis.
What is Mast Cell Activation Syndrome (MCAS)?
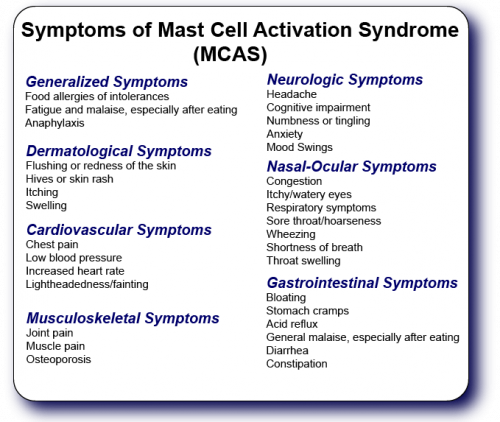
Mast cell activation syndrome (MCAS) is a disorder of the mast cells that causes them to release an overabundance of mediators. This release is often in response to non-life-threatening conditions. This abundant release triggers widespread inflammation in the body, resulting in a wide variety of symptoms that can affect multiple systems in the body. These symptoms are not just limited to typical allergic responses.
MCAS can affect multiple systems throughout the body, causing a widespread list of possible symptoms.
Diagnosing MCAS
Diagnosing MCAS comes with a variety of different challenges. In most cases, patients see their physicians when they are not experiencing symptoms or in the middle of an episode. The chemicals released by the mast cells only circulate in the body for a short time, making laboratory diagnosis difficult to obtain. For example, total serum mast cell tryptase must be drawn between 30 minutes and two hours after the start of an episode and a 24-hour urine must be started immediately after the start of an episode.
In some cases, physicians may order blood and urine tests, as well as tissue biopsies. In most cases, physicians diagnose MCAS through medical history, a collection of symptoms, and how the patient responds to initial treatment options.
Treatment of MCAS
The goal of initial treatment for MCAS is two-fold. The immediate goal is to address and improve symptoms and quality of life. Secondly, the initial treatment works as a diagnostic tool. If a patient does not respond to an initial treatment of histamine type 1 receptor blockers, such as diphenhydramine and hydroxyzine, chances are they do not have MCAS and are suffering from another condition. Once MCAS is confirmed through a positive response, other treatment options focus on improving symptoms and reducing flare-ups of MCAS symptoms.
Medications for the Treatment of MCAS
Medications, as we mentioned, provide symptom relief and act as a diagnostic tool in the beginning. Some common MCAS medications include:
- Emergency Medications – Adrenaline-based interventions, such as epinephrine (EpiPens) open the airways and work to address anaphylaxis.
- Mast cell stabilizers – Medications, such as ketoifen and sodium cromoglicate, stabilize mast cells and reduce the release of mediators.
- Mediator blockers – Mediator blockers, such as H1 and H2 antihistamines (diphenhydramine, loratadine, ranitidine, or famotidine), anti-leukotrienes, and anti-prostaglandins, help block the effects of mast cell mediators.
- Corticosteroids – Corticosteroids, such as prednisone, help to reduce inflammation.
- Vitamin & Mineral Supplements – Vitamins, such as vitamins C & D, Magnesium, and probiotics contribute to mast cell stabilization, preventing inflammatory responses, and the production, regulation, and breakdown of histamines.
- Omalizumab – This medication blocks the binding of IgE to receptors and helps reduce mast cell reactivity and sensitivity, helping to reduce the risk of anaphylactic reactions.
Low Histamine Diet
Many people with MCAS may find that eating certain foods can trigger symptom flares. This is because many foods we eat contain natural histamines that, when ingested, can trigger symptoms. Physicians may suggest a low histamine diet as a possible solution. However, do not attempt this type of diet on your own, as it can lead to malnutrition. A registered dietician can help you develop a diet plan that reduces your histamine intake while still meeting your nutritional needs.
For many patients, keeping a food diary can be beneficial. Make note of any foods that may seem to trigger symptoms and let both your physician and dietician know what these foods are.
Foods High in Histamines
- Alcoholic beverages
- Eggplant
- Pickled or canned foods
- Matured cheeses
- Smoked meat or lunch meats (salami, ham, sausage, etc.)
- Shellfish
- Beans
- Long-stored nuts (peanuts, cashews, almonds, pistachios)
- Chocolate and cocoa-based products
- Pre-made meals (TV dinners)
- Salty snacks
- Anything with preservatives and artificial colorings
- Processed foods
Foods Low in Histamines
- Fresh meats
- Fresh fish
- Cream cheese, butter, and mozzarella cheese
- Fresh chicken
- Eggs
- Fresh fruits, with the exception of plantains and citrus (citrus foods are considered histamine releasers)
- Fresh vegetables, with the exception of tomatoes, eggplant, and spinach
- Grains
- Fresh pasteurized milk
Common MCAS Comorbidities
Studies on MCAS have found correlations with many other medical conditions. In many cases, it is unclear whether the MCAS predates the other conditions or if the other conditions triggered the MCAS. Some common comorbidities seen with MCAS include:
- Postural orthostatic tachycardia syndrome (POTS)
- Myalgic encephalomyelitis/chronic fatigue syndrome
- Ehlers-Danlos syndrome (EDS)
- Irritable bowel syndrome (IBS)
- Fibromyalgia
- Cancer
- Complex regional pain syndrome (CRPS)
- Neuropsychological conditions (autism, anxiety, and depression)
- Epstein-Barr virus (EBV)
- Thyroid disease
- Celiac disease
- Sickle cell disease
MCAS and Long COVID
Many Long COVID patients are also being diagnosed with MCAS. However, it is unknown currently if the SARS-CoV-2 virus triggers mast cell dysfunction or if an underlying mast cell dysfunction contributes to the development of Long COVID. Researchers believe that the SARS-CoV-2 virus increases activation of the mast cells, resulting in the symptoms many see with Long COVID. If this is the case, possible MCAS treatments, such as H1 and H2 mediator blockers, may prove to be an effective therapy for both MCAS and Long COVID.

Get updates
Join our mailing list