Now live! RTHM Direct – simplified medication access for Long COVID, ME/CFS and related conditions. Check it out
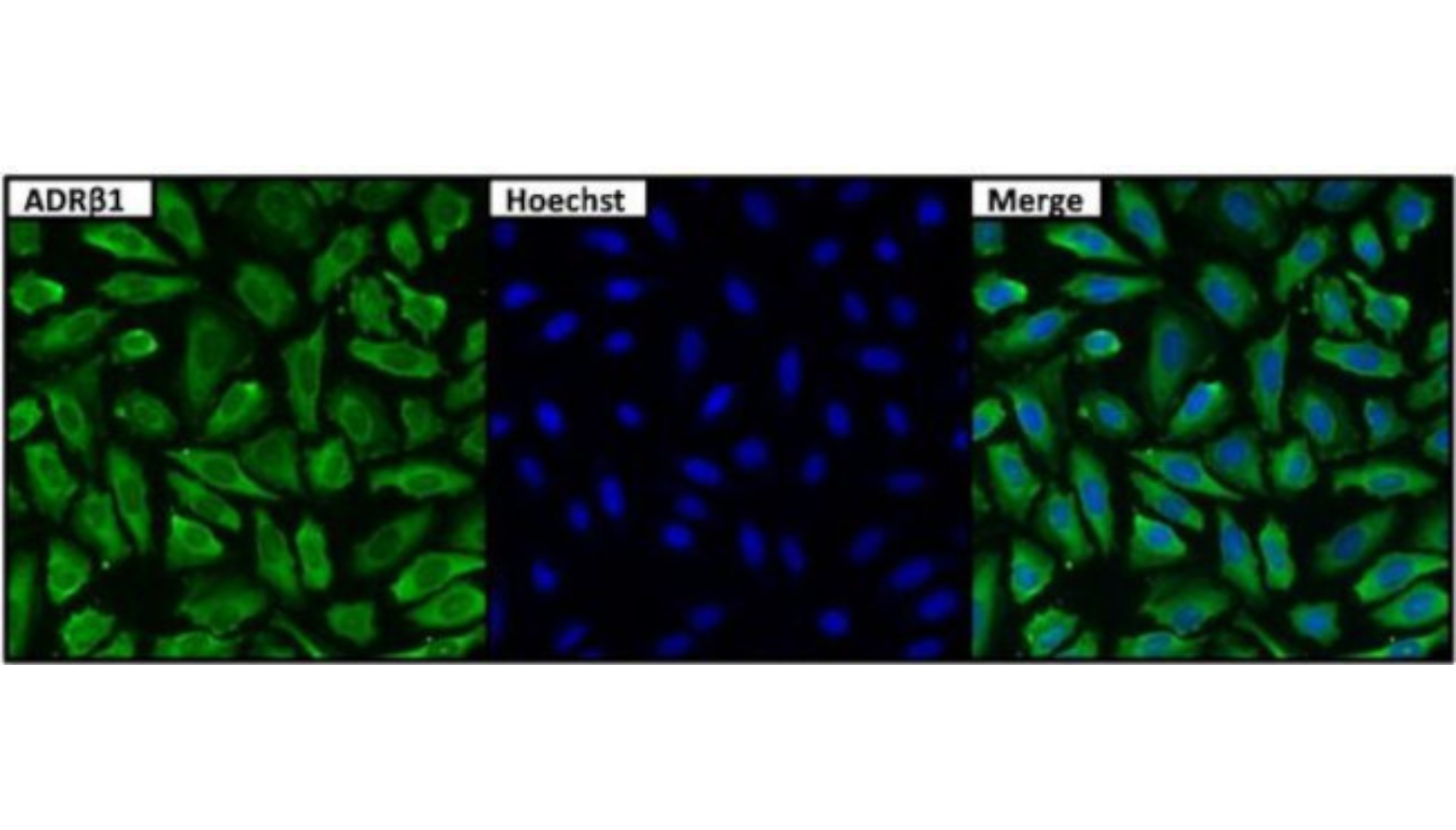
The β1-adrenergic receptor (β1-AR) is a G protein-coupled receptor. The β1-AR plays a crucial role in mediating the positive inotropic (strength of contraction) and chronotropic (rate of contraction) effects on the heart in response to catecholamines, especially noradrenaline and adrenaline. Agonist binding causes a rise in the intracellular concentration of the second messenger cAMP. The anti-β1-adrenergic-receptor-antibody EIA is designed for the determination of antibodies (IgG) against the β1-adrenergic receptors (β1-AR) in serum and plasma.
Theoretically, binding of an antibody to this receptor could result in activation or inhibition of its function, leading to increased or decreased cardiac output (the amount of blood the heart pushes out), changes to heart rate and strength of contraction, changes to muscle contractility of the bladder, glucose metabolism, circadian rhythm regulation, amongst many other potential issues.
Autoantibodies to β1-adrenergic receptors (β1-AR)
The effects of autoantibodies on β1-adrenergic receptors (β1-AR) have been primarily associated with cardiovascular diseases. However, there is evidence of autoantibodies against β1-adrenergic receptors in connection with Postural Orthostatic Tachycardia Syndrome (POTS), Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS), and Long COVID. These autoantibodies can affect the function of the β1-adrenergic receptors, leading to dysregulation of the autonomic nervous system and contributing to the symptoms experienced by individuals with these conditions.
Postural Orthostatic Tachycardia Syndrome (POTS)
There is evidence suggesting a connection between autoantibodies against β1-adrenergic receptors and conditions such as postural orthostatic tachycardia syndrome (POTS). Autoantibodies to β1-adrenergic receptors can lead to an overstimulation of these receptors, resulting in symptoms such as rapid heart rate, dizziness, and fatigue. Studies have shown the presence of these autoantibodies in patients with POTS. However, more research is needed to fully understand the role of these autoantibodies in these conditions and their potential as diagnostic markers or therapeutic targets. (Li et al. 2014)
In a study, immunoglobulin G (IgG) derived from POTS patients was found to activate β1-adrenergic receptors (β1AR) in cell-based assays. (Fedorowski et al. 2018)
Another study found that patients with POTS had elevated levels of autoantibodies against the adrenergic alpha 1 receptor (α1AR) and β1AR. (Gunning et al. 2020)
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
Autoantibodies against β1-adrenergic receptors have been found to be elevated in patients with Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS). These autoantibodies are potential biomarkers for ME/CFS and may play a role in the pathogenesis of the disease. Studies have shown a significant increase in β1-adrenergic receptor autoantibodies in ME/CFS patients compared to healthy controls. Additionally, the levels of these autoantibodies have been found to correlate with immune markers and disease severity in ME/CFS patients. Further research is needed to fully understand the role of β1-adrenergic receptor autoantibodies in ME/CFS. (Loebel et al. 2016) (Fujii et al. 2021) (Bynke et al. 2021)
Cardiovascular Conditions
Autoantibodies against β1-adrenergic receptors (β1-AR) have been implicated in various cardiac conditions. These autoantibodies can activate β1-AR, leading to altered cardiac function and potentially contributing to the pathogenesis of dilated cardiomyopathy (DCM), heart failure, and other heart diseases.
In patients with dilated cardiomyopathy, approximately 25% have activating autoantibodies against human β1-AR. These autoantibodies impair receptor-ligand binding and enhance receptor-mediated signaling, which can be counteracted by β-adrenergic receptor blockade. The presence of these autoantibodies is associated with poorer left ventricular function. (Jahns et al. 1999)
The imbalance between β1-AR autoantibodies and β2-AR autoantibodies may also play a role in cardiac structure and function. An increased ratio of β1-AR autoantibodies to β2-AR autoantibodies is associated with worsening heart failure. β2-AR autoantibodies can antagonize the effects of β1-AR autoantibodies, providing a potential therapeutic target. (Cao et al. 2019)
In addition to heart disease, β1-AR autoantibodies have also been implicated in other conditions. For example, they have been found in patients with chronic Chagas heart disease, a chronic manifestation of Trypanosoma cruzi infection. These autoantibodies can bind to native human β1-AR and have an agonist-like effect, contributing to the pathogenesis of the disease. (Labovsky et al. 2007)
It is important to note that the clinical significance and prevalence of β1-AR autoantibodies in human heart disease are still not fully understood. Further research is needed to determine the true prevalence, clinical impact, and events triggering their production. Reliable detection of these autoantibodies is crucial for potential diagnostic and therapeutic strategies. (Bornholz et al. 2015)
Learn more about autoantibody testing at “RTHM Lab Now Offering GPCR+ Autoantibody Panel” and visit our Lab Page to order your GPCR+ Antibody Panel today.
Featured image courtesy of ThermoFisher Scientific

Get updates
Join our mailing list