Now live! RTHM Direct – simplified medication access for Long COVID, ME/CFS and related conditions. Check it out
The arrival of the SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2) virus in 2019 brought a lot of uncertainty and many questions for both physicians and the general population. As the COVID virus spread, positive cases, hospitalizations, and deaths rose quickly. While many have since recovered, others are facing an additional complication of the SARS-CoV-2 virus: Long COVID. Long COVID, also known as PASC (Post-Acute Sequelae of SARS-CoV-2 Infection), refers to the continuing, reoccurring, or new long-term symptoms that occur in patients already recovered from an initial acute COVID infection.
RTHM, led by Chief Medical Officer Jennifer M. Curtin, MD, is here to provide treatment and education for those experiencing general symptoms of Long COVID, suffering from common comorbidities, or taking care of someone experiencing these symptoms. The battle against Long COVID has just begun, but here at RTHM we understand what it is like to live with disabling conditions that are often overlooked or misunderstood, and the team at RTHM is here to let you know you are not alone!
What is Long COVID?
Most people infected with COVID recover from their symptoms within 4 weeks of initial onset. Unfortunately, that is not the case with everyone. A wide range of patients go on to experience lasting symptoms, as well as develop additional symptoms. This is true even when their initial COVID case was minimal or asymptomatic. In fact, the current estimate is that 10-15% of patients testing positive for COVID will experience Long COVID.
Post COVID-19 condition occurs in individuals with a history of probable or confirmed SARS CoV-2 infection, usually 3 months from the onset of COVID-19 with symptoms that last for at least 2 months and cannot be explained by an alternative diagnosis. Common symptoms include fatigue, shortness of breath, cognitive dysfunction but also others and generally have an impact on everyday functioning. Symptoms may be new onset following initial recovery from an acute COVID-19 episode or persist from the initial illness. Symptoms may also fluctuate or relapse over time.
The Different Categories of Long COVID
Long COVID is broken down into three distinct categories based on symptoms and the timing of symptom development.
- Category 1
The first category of Long COVID is for those patients experiencing continuous symptoms of their initial COVID infection. The SARS-CoV-2 virus causes direct cell damage and this damage results in lingering and long-lasting symptoms. - Category 2
This category covers those with post-ICU care syndrome, and this affects those patients who required ICU hospitalization for their COVID treatment. - Category 3
The 3rd category is for those patients who experience the return of COVID symptoms or new symptoms after their initial recovery from an acute infection. From what we are learning, no organ system is spared from the effects of the virus, and these symptoms can vary immensely. In addition, there is currently no risk factor understanding, with Long COVID affecting men, women, and children of all ages. The severity of your initial COVID-19 infection does not determine your risk of developing Long COVID.
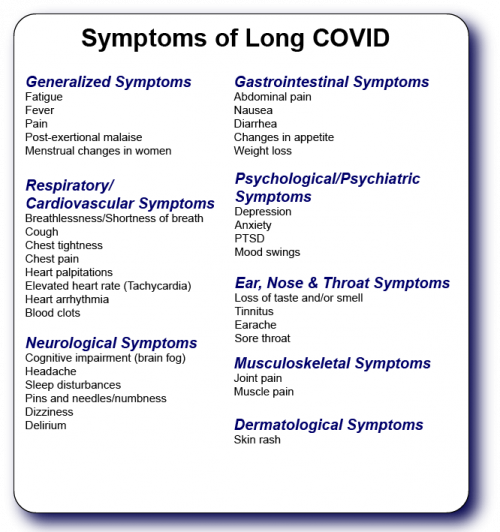
Symptoms of Long COVID
Symptoms of Long COVID can affect every system in the body and patients can have a wide variety of symptoms. These symptoms can also change over time. Every patient is unique in their symptoms. The three most common symptoms include fatigue and exertional intolerance, cognitive complaints (brain fog), and non-restorative sleep.
For a More In-Depth Look at Long COVID, Click HERE
Long COVID Comorbidities
Some people with Long COVID go on to be diagnosed with other, often viral-associated diseases. Similar conditions have been seen in survivors of both Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS). Unfortunately, many of these patients still show symptoms and organ damage at the 7–15-year mark.
In addition to the symptoms mentioned above, many Long COVID patients are developing additional comorbidities, seemingly triggered by the SARS-CoV-2 virus and subsequent infection. The most common conditions seen include ME/CFS, POTS, MCAS, autoimmunity, and small fiber neuropathy. It is important to address any symptoms due to these conditions as they arise.
Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS)
Myalgic encephalomyelitis/chronic fatigue syndrome, or ME/CFS, is a complex multi-system illness that frequently onsets after a stressor. This stressor is frequently a viral illness. ME/CFS is a serious, chronic, and often debilitating disease that affects multiple body systems. This includes the nervous system, immune system, and the ability of the body to produce energy.
Unfortunately, there is still much that researchers and physicians do not understand when it comes to ME/CFS, but they do know it is not due to deconditioning. Because there is no single, diagnostic biomarker for ME/CFS, and medical education on the condition is sparse, diagnoses can be challenging to access.
Common symptoms seen with ME/CFS can include, but are not limited to, the following:
- Post-exertional malaise (an unusual response to physical or cognitive effort)
- Extreme exhaustion
- Confusion and cognitive impairment
- Non-restorative sleep or reversed diurnal rhythm (sleepy during the day, wakeful at night)
- Dizziness and lightheadedness
- Orthostatic Intolerance – abnormal response to being upright, causing dizziness, fainting, or other symptoms that resolve when sitting or lying down.
- Elevated heart rate (tachycardia)
- Lymph node tenderness
- Headaches of new origin
- Muscle pain
- Joint pain
- Sensitivities to light, sounds, or chemicals
- Inability to regulate body temperature
- Extreme thirst and frequent/excessive urination
- Gastrointestinal issues
Diagnostic Criteria for ME/CFS
Diagnosis currently relies on specific diagnostic criteria that include three main symptoms and at least one of two additional manifestations:
Mandatory Three ME/CFS Symptoms
- Post-exertional malaise (unusual symptoms after physical or cognitive effort)
- Unrefreshing sleep
- A substantial reduction in the ability to engage in pre-illness levels of occupational, educational, social, or personal activities that persist for more than 6 months and is accompanied by fatigue not alleviated by rest.
One of the Two Following Must Also Be Present
- Cognitive Impairment
- Orthostatic Intolerance
For a More In-Depth Look at ME/CFS, Click HERE
Dysautonomia, Including Postural Orthostatic Tachycardia Syndrome (POTS)
Dysautonomia is a broad term used to cover a variety of different medical conditions that cause a malfunction to occur in the autonomic nervous system (ANS). The autonomic nervous system controls automatic regulatory processes within the body, such as heart rate, blood pressure, digestion, breathing, and temperature control. While the most common form of dysautonomia is Neurocardiogenic Syncope (NCS), the form of dysautonomia most seen in patients with Long COVID is postural orthostatic tachycardia syndrome (POTS).
POTS is a form of orthostatic intolerance, meaning difficulty tolerating changes that occur when a person moves from lying down to a sitting or standing position. POTS is diagnosed by measuring changes in heart rate with changes in position. People with POTS may experience this as a feeling of their heart pounding, racing, or feeling dizzy when standing up or standing still. Additional symptoms can include:
- Fatigue
- Headaches
- Lightheadedness
- Heart palpitations
- Exercise intolerance
- Nausea
- Brain fog
- Fainting
- Cold and/or painful extremities
- Chest pain
- Shortness of breath
- Livid or blotchy legs
- Bulging veins in hands or feet
- Poor Blood Circulation
- Numbness
- Irritable Bowel Syndrome
- Blurred Vision
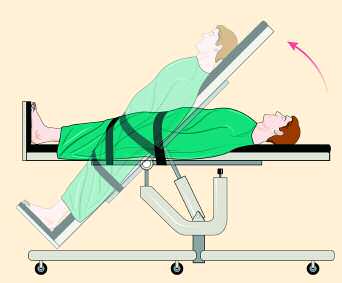
Diagnostic testing for POTS typically involves the use of a Tilt Table Test that measures changes in heart rate and blood pressure as a person is gradually tilted from the supine (lying down) position to that of nearly standing. Criteria for a POTS diagnosis include a heart rate increase of 30 beats per minute or more, or a heart rate over 120 bpm, within the first 10 minutes of upright tilt, without the presence of orthostatic hypotension (decrease in blood pressure). Other tests often used in diagnosis include the Quantitative Sudomotor Axon Reflex Test (QSART), Thermoregulatory Sweat Test, gastric motility studies, and skin biopsies that look at the small fiber nerves.
For a More In-Depth Look at POTS, Click Here
Mast Cell Activation Syndrome (MCAS)
Mast cells are a type of white blood cell found throughout the body. These cells play an important role in the body’s immune response. The cells contain mediators of immune function, such as histamines and cytokines that they may release in response to changes in their environment. This release causes symptoms such as itching and flushing, but in more severe cases, can lead to anaphylaxis. In a healthy body, these mast cells are beneficial and play a vital role in immune function.
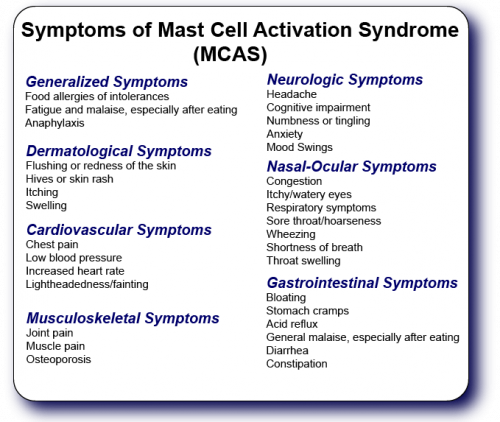
Mast cell activation syndrome (MCAS) is a disorder of these mast cells, causing them to release an abundance of these mediators, often in response to triggers that are not life-threatening. This inappropriately triggered inflammation in the body can lead to a wide variety of different symptoms, affecting multiple systems in the body, and these symptoms are not limited to simple allergy symptoms.
Diagnostic Testing and Criteria for MCAS
Currently, receiving a diagnosis for MCAS can take time, and finding the right doctor. Unfortunately, the blood and urine tests that can measure these mediators must occur during an episode when the mediators are released. This means routine testing often does not pick up potential markers and makes a laboratory diagnosis difficult to obtain. In most cases, physicians work to eliminate potential underlying conditions and make a diagnosis based on medical history, symptoms, and reactions to traditional MCAS treatment options. Unfortunately, MCAS is another medical condition that most physicians never learn about and is not on the radar for most, meaning you will likely need to find a physician specializing in MCAS in order to receive a diagnosis.
For a More In-Depth Look at MCAS, Click HERE
Autoimmunity
In a healthy immune system, an antigen (virus or bacteria) enters the body and triggers immune cells to produce antibodies. These antibodies attach to the antigen and signal the immune system to target and destroy it. In autoimmunity, this system malfunctions, and a person’s body produces autoantigens or self-antigens. In this case, the body responds with autoantibodies that attack healthy cells in the body. This immune response leads to conditions such as rheumatoid arthritis, lupus, Sjogren’s, and a wide range of other autoimmune conditions.
In many cases, studies have shown that viral and bacterial infections can trigger autoimmunity conditions in patients and, according to recent signs, SARS-CoV-2 is no different. But how can a virus trigger an autoimmune response? When a virus, like SARS-CoV-2, enters the body, it relies on the body’s cells to copy itself and spread. As it does this, the virus can alter the amounts, locations, and binding partners of normal human proteins. This alteration can trigger the immune system to see these proteins as foreign and begin targeting them, resulting in autoimmune symptoms and conditions. Early studies are showing a possible connection between these autoantibodies and Long COVID.
For More In-Depth Information on Autoimmunity, Click HERE
Small Fiber Neuropathy
Small fiber neuropathy, often referred to as autonomic neuropathy, occurs when the small nerves in the body responsible for sensations, breathing, heart rate regulation, perspiration, and digestion sustain damage. This damage can occur due to a variety of medical conditions, such as diabetes, injuries, infections, and some vitamin and mineral deficiencies. However, in some patients, an underlying cause is never identified. Pain in the feet and hands is often the first symptom of small fiber neuropathy, but other symptoms can include:
- Paresthesia – a tingling or prickling sensation
- Hypersensitivity to touch and temperature changes
- Numbness in the feet, legs, or lower abdominal region
- Bladder control issues
- Constipation
- Sexual dysfunction
- Excessive or infrequent sweating
- Skin discoloration
- Dry eyes and mouth
- Low blood pressure can contribute to fainting
- Rapid or irregular heartbeat
Diagnosing Small Fiber Neuropathy and Its Connection to COVID
In terms of general diagnostic testing for small fiber neuropathy, physicians often order electromyography and nerve conduction studies to eliminate the involvement of large nerve fibers. A skin biopsy then looks for and confirms small fiber damage.
In terms of small fiber neuropathy in connection with Long COVID, a small study published in the British Journal of Ophthalmology shows the answer may be in the eyes. Physicians have used a non-invasive, high-resolution imaging laser test, known as corneal confocal microscopy (CCM), to identify nerve damage and inflammatory changes for a variety of different medical conditions, such as diabetic neuropathy and fibromyalgia. For patients with suspected Long COVID with the presence of small fiber neuropathy symptoms, this test can confirm the small fiber loss, as well as increased dendritic cells, which play an active role in the body’s immune response.
For More In-Depth Information on Small Fiber Neuropathy, Click HERE
Treatment of Long COVID and Comorbidities
Long COVID is different for every individual and because it is a multi-system condition, treatment requires the expertise of many different medical specialists. For this reason, Long COVID clinics such as RTHM are bringing together physicians from many different specialties. This allows us to provide every patient with individualized and coordinated care specific to the symptoms and complications they are facing.
When You Can’t Find Answers
Are you still suffering symptoms months after your initial COVID diagnosis? Did you recover from COVID only to develop new symptoms 3-4 months later? Have you watched everyone around you recover only to be stuck with symptoms that just will not go away or even improve? Have you been unable to get answers from your primary care provider? If you answered yes to any of these questions, you are not alone. Unfortunately, many Long COVID patients are not receiving the care and answers they are looking for from the general medical community and, instead, turn to their own research looking for answers. This is how organizations like Body Politic’s COVID community developed. Patients struggling to find answers came together with medical professionals and researchers to help those battling Long COVID.
Through a global network of COVID-19 patients, chronic illness allies, and health and disability advocates, Body Politic breaks down barriers to patient-driven whole-person care and well-being, particularly for historically marginalized communities by facilitating peer-support, cultivating patient-led research and public education, and leading community-based advocacy.
Thanks to the actions of patients and groups like these, many patients are finding answers and treatments for Long COVID. Long COVID clinics, like RTHM, are finally providing patients who have felt lost with Long COVID some much-needed answers, treatments, and support.
Treatment Begins with an Accurate Diagnosis Via Conservative Diagnostic Testing
If you are experiencing what you believe may be Long COVID, a visit to an RTHM primary care physician is your first step. They are often able to diagnose many of the Long COVID symptoms based on your medical history and a physical exam. In some cases, symptoms may require additional testing. However, CDC Long COVID Care Considerations recommend a conservative approach to diagnostic testing during the first 4-12 weeks of symptoms, as many laboratory and imaging studies often show normal or nondiagnostic results and symptoms may resolve on their own. Unfortunately, not enough is known about Long COVID to ensure one test will diagnose the disease. However, testing may be necessary to diagnose conditions that the SARS-CoV-2 virus may have triggered. If symptoms persist for more than 3 months, further evaluation and testing are often necessary.
Customized Treatment Plans Based on Symptom Presentation
The goal of treatment is to optimize the patient’s functional abilities and quality of life by addressing and managing symptoms and comorbidities, such as ME/CFS and POTS.
As a patient, keeping a journal of your symptoms, the severity of symptoms, and a relationship with potential triggers (exercise, foods, menstruation, etc.) can provide your physician with a greater insight into your health and provide the insights needed to adjust your treatments as necessary.
Comprehensive Coordinated Care for Treatment
Because patients with Long COVID often have symptoms affecting a wide range of organs and systems, care typically requires a coordinated effort between specialists, such as neurologists, cardiologists, pulmonologists, psychologists, and nutritionists. This is where specialized Long COVID clinics, such as RTHM, offer more comprehensive care. The physicians in these clinics specialize in Long Covid and are following new developments in the SARS-CoV-2 pandemic and treatments for Long COVID. This means they better understand their Long COVID patients and are able to provide cutting-edge solutions.

Get updates
Join our mailing list