Now live! RTHM Direct – simplified medication access for Long COVID, ME/CFS and related conditions. Check it out
Caring for a loved one with ME/CFS or Long COVID can be challenging. As a caregiver, it is our role to not only care for our loved ones but also to act as a mediator and advocate in every aspect of life. This includes the often challenging discussion with friends, family, colleagues, and even medical professionals about the life-altering illness that we and our loved ones face every day. Here the team at RTHM and Kim Moy from Caregiver Wisdom join together to offer suggestions for caregivers to discuss your loved one’s illness, the limitations that affect both you and your loved one, and how they can lend an understanding ear and helping hand if they are willing.
Starting the Conversation on ME/CFS or Long COVID as a Caregiver
Caregivers can play a vital role in mediating and helping our loved ones who struggle with the highly emotional aspect of discussing their illness with family and friends. As a caregiver, discussing the illness may come up when you have to cancel get-togethers, when you’re not able to accept invitations in the first place, when you field questions from friends and family about changes they observed, or when they insinuate something, such as “XYZ should really start pulling their weight.”
When approaching a discussion about your loved one’s illness, there are specific factors to consider.
- Who are you talking to? Are you talking with a family member, close friend, or acquaintance like a neighbor, work colleague, or a doctor?When talking with someone you are close to and feel comfortable with, you may decide to share more details. When talking with an acquaintance or a work colleague, you are more likely to share less unless they ask questions and seem genuinely interested in learning more. When talking with a doctor, consider asking how much they already know about ME/CFS/Long COVID before deciding what additional information to share with them.
- How much time and how in-depth do you want to go? Consider developing a standard 30-second version that hits the main points. Give this short version first, and then if the person has questions or shows more interest, add more details.
- Do you anticipate disbelief, denial, rejection, or belittling? Depending on the situation and your relationship with the person, you can quote facts from sources like other RTHM content, the U.S. Centers for Disease Control (CDC) ME/CFS and Long COVID webpages and the Mayo Clinic. Or you can decide to minimize your contact with this person. It’s important to pick your battles to preserve your own mental health.
Sample Scenarios for Caregivers to Consider When Sharing about ME/CFS and Long COVID
Talking to others about your loved one’s illness can be difficult. How much should you share? What information is important? Oftentimes, it is a good idea to have an internal script ready that allows you to touch on vital information and be prepared if there are additional questions. Here we look at different scenarios and what you might choose to share.
Talking with Friends and Family
Here is a 30-second script that you can customize to your loved one’s specific illness and situation.
My (partner/child/friend) has a debilitating illness called Myalgic Encephalomyelitis. (You can also include that it’s also known as Chronic Fatigue Syndrome, but this can detract from the severity of the illness and often triggers responses like “Oh yeah, I’m tired too,” which is super annoying.)
I know it’s a mouthful. It technically means “muscle pain, and brain & spinal cord inflammation.” It’s a neurological illness that causes a lot of pain, fatigue, unrefreshing sleep, and brain fog. My (partner/child/friend) hasn’t been able to work/go to school/get out of bed for the past xx years. A lot of people with Long COVID are now suffering from the same problems and many doctors and scientists think they may be the same illness triggered by different viruses.
If people seem interested in learning more, you can add additional descriptions.
- Some people say it’s like you’re a battery and you can never get fully charged to 100% no matter how much sleep & rest you get. Depending on the person and if they’re having a good day or bad day, it’s like you have only 20-50% of your battery to operate from.
- It’s like having a constant flu that you can’t get rid of.
- There are actually up to 200 different symptoms that people can get. It’s a very debilitating illness that can affect multiple systems in your body: the brain, immune system, heart, lungs, nervous system, GI, and more.
- Some people who have it are housebound or even bedbound. People who have it the worst can’t even talk and need to lie down in dark rooms.
If they are interested and want to learn more, have resources available to share with them. Some great resources include:
- Mayo Clinic’s Concise Review for Clinicians: Diagnosis and Management of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
- “Unrest” Documentary
- “Fatigue Can Shatter a Person”
- “What Makes Brain Fog So Unforgiving”
- “What Does Brain Fog Feel Like?”
- “Long COVID Has Forced the U.S. to Take Chronic Fatigue Syndrome Seriously”
- Diagnosing and Treating Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) by the U.S. ME/CFS Clinician Coalition (July 2020)
- Bateman Horne Center Educational Resources
Talking with Managers and Colleagues
It’s a personal decision on whether to share your loved one’s illness with your manager and/or colleagues at work. In some cases, you may feel you’re jeopardizing what people think of you and your capacity to take on more challenging assignments, which can limit your career growth. In other cases, you may want to share with your manager and your immediate team so they understand that you need to take your loved one to doctor’s appointments and/or need to work from home once in a while.
Kim Moy shares:
When interviewing for jobs in the past, I would wait to get the job offer and then tell the hiring manager that I was excited about the opportunity to join the team and wanted to ask about job flexibility. I’d then say that my spouse has a debilitating illness called ME, give a few brief bullet points to describe it, and then say that job flexibility is important to me so I can take my partner to occasional doctor’s appointments while also making sure I get my work done.
At my last job, I also asked for the ability to work from home two days per week, even before COVID hit. My hiring manager said OK to a partial work-from-home schedule when I told her that I’ve successfully managed remote employees in other regions of the world at previous jobs. (When COVID hit and we all had to work from home, I and others on my team were able to successfully negotiate to become 100% remote employees. Several people – including me – even moved across the country to live in places with a lower cost of living and slower pace of life for a healthier lifestyle for our families. If you are able to get a remote job, it can offer more job flexibility and no wasted time commuting.)
Talking with Physicians
Unfortunately, ME/CFS, Long COVID, chronic Lyme and other debilitating infectious-related chronic illnesses are poorly understood and/or under-researched. This is especially true when standard tests come back normal. In addition, Many medical students do not learn much more than a single lecture or less on these conditions during their training, so the average primary care physician may not understand these conditions at all.
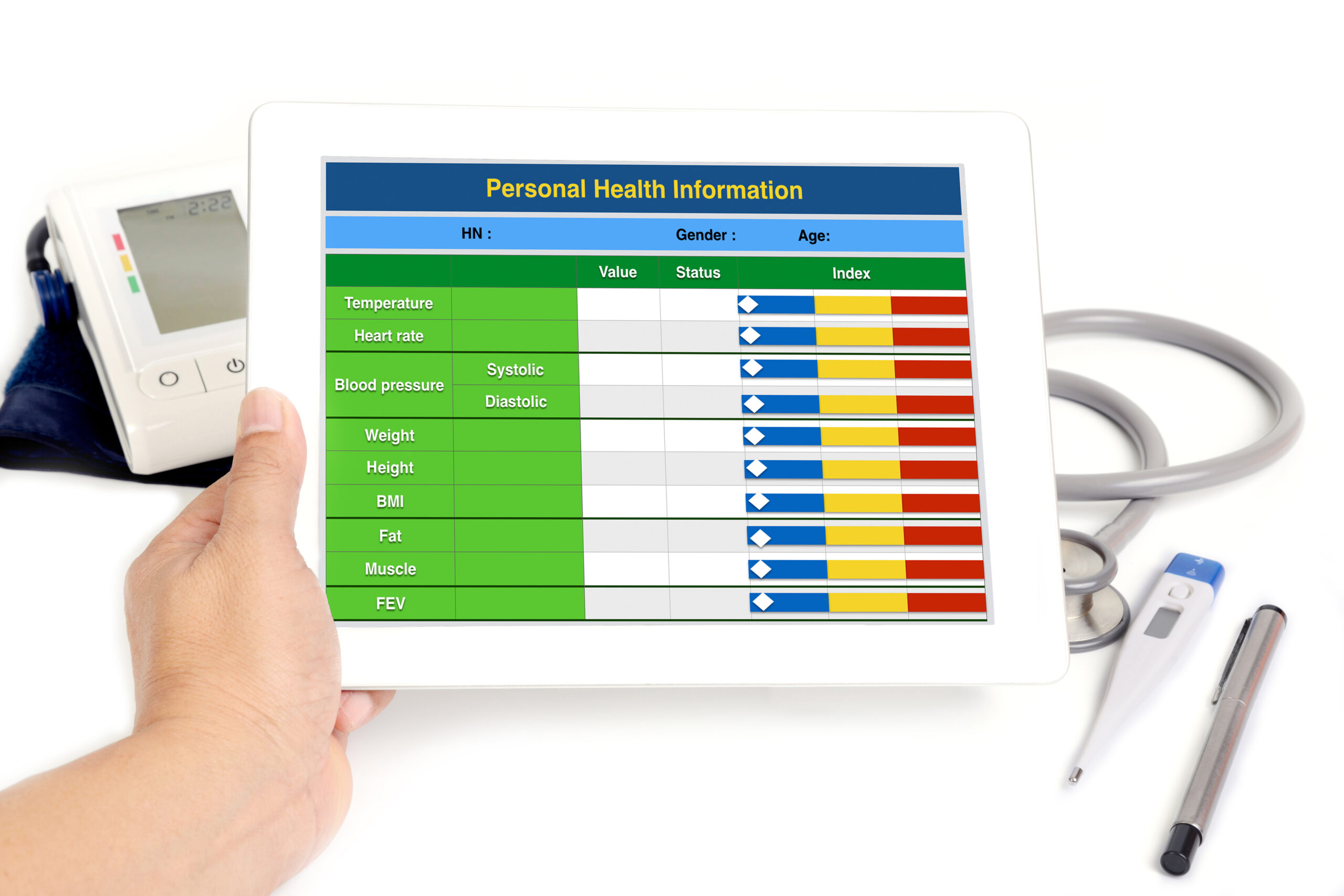
In these scenarios, it is important that, as a caregiver, you help ensure that the physicians treating your loved one are aware of the illness and how it affects day-to-day life. Some resources to help you achieve these goals can include everything from providing specific illness information from reputable sites to compiling a health summary and medical journal to show the direct effects of the illness on your loved one. The following references offer additional information and support when it comes to talking with healthcare professionals.
- Partnering with Your Medical Team
- Creating a Health Snapshot Sheet
- How to Compile a Comprehensive Personal Health Record
- How to Create a Symptom and Activity Tracker
- Mayo Clinic’s Concise Review for Clinicians: Diagnosis and Management of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome
When People Offer to Help
If someone asks how they can help, or if you want to proactively bring it up, you can identify ways family and friends can support you/your family. It’s great to be prepared to list a few ways they can support you and your loved one.
For example, if you have young kids and a chronically ill partner, you can say “It’s tough to be stretched thin and running around taking care of everything, so sometimes it’s nice when my son/daughter can hang out with their friends for a few hours or for a day so I can get a break. Do you think my son/daughter can have a playdate or hang out with your son/daughter at your house once in a while?”
When Responses Are Disheartening
We have all heard the typical “Oh yes, I get tired too!” or “Have you tried yoga or XYZ treatment?” or “Oh yes, my friend has that condition but got better with XYZ!” Hearing these comments from friends, family, coworkers, and even healthcare professionals can be disheartening. So, what do you do when you get hurtful reactions from well-meaning family or friends, or when family, friends, or insensitive physicians do not believe you?
First off, you may want to pick your battles. Ask yourself if it’s worth the extra effort or do you want to just move on? That said, sometimes we struggle with what to say, and it’s helpful to have some quick responses in your back pocket if you want to use them.
Also, if they are trying to be empathetic and well-meaning (but grasping at what to say), you may want to start off by acknowledging it and say “Thanks, I appreciate your concern.”
Common comments you may hear:
- “Oh yes, I get tired too!” A suggested response for you: “This is something different. It’s a deeper level of fatigue that you can’t recover from with just sleep and rest.”
- “Have you tried XYZ?” A suggested response from you: “Thanks, we’ve tried that, and unfortunately not all treatments work for everyone the same way.”
- “You should exercise more.” A suggested response from you: People with M.E. suffer from what’s called post-exertional malaise. It means you’re wiped out after you use too much energy. It’s important to pace yourself and closely manage your energy levels.
- Perhaps you’re dealing with a family member or friend who is persistent in offering advice and doesn’t believe the illness is a long-term debilitating condition. A suggested response from you: “Thanks for your concern. We’re doing the best we can.” Then let it roll off of you and maybe change the topic.
- “I hope xxx feels better soon.” A suggested response from you: “Thanks, we’d love for xxx to be better. Chronic illness is an ongoing battle that takes constant management.”
If the conversation is upsetting, you may want to reach out to family or friends who understand or talk about it with a caregiver support group for ME/CFS, Long COVID, and related illnesses.
Importance of Informing Others
By openly sharing this information, caregivers can help raise awareness and foster empathy. First, these conditions aren’t well understood and many people aren’t familiar with the debilitating symptoms and the impact they have on a person’s life. Sharing the diagnosis with others could lead to a more accommodating and inclusive situation, where social gatherings and plans can be adapted to the patient’s energy levels and specific needs. It also encourages open communication, making it easier for friends to offer help when necessary so that your loved one does not feel as isolated or misunderstood. Ultimately, informing others about the illness can help build a compassionate community that provides support to you and your loved one.
If you’re looking for medical care for chronic illnesses like ME/CFS and Long COVID, RTHM has a telehealth care team specializing in treating these complex health conditions.
For more chronic illness caregiving advice, Caregiver Wisdom has blog posts and other resources.

Get updates
Join our mailing list