Now live! RTHM Direct – simplified medication access for Long COVID, ME/CFS and related conditions. Check it out
Pain, whether from an injury or a medical condition, can affect many aspects of daily life. If you break an arm, you can expect pain at the sight of the injury and limited use of the arm. But as the bone heals, the pain eases and you slowly regain normal function. Fibromyalgia, however, is a chronic disorder that causes unexplained widespread pain and tenderness throughout the body.
Here we dive into fibromyalgia and what we know about this chronic condition, the symptoms associated with this condition, the potential treatment options, and what we are learning about the connection to those with Long COVID and ME/CFS.
What Is Fibromyalgia?
Fibromyalgia, often referred to simply as “fibro,” is defined as a chronic disorder characterized by widespread musculoskeletal pain and tenderness throughout the body. The term “fibromyalgia” comes from the Latin “fibro,” meaning fibrous tissues, “my” referring to the muscles, and “algia” referring to pain.
History of Fibro
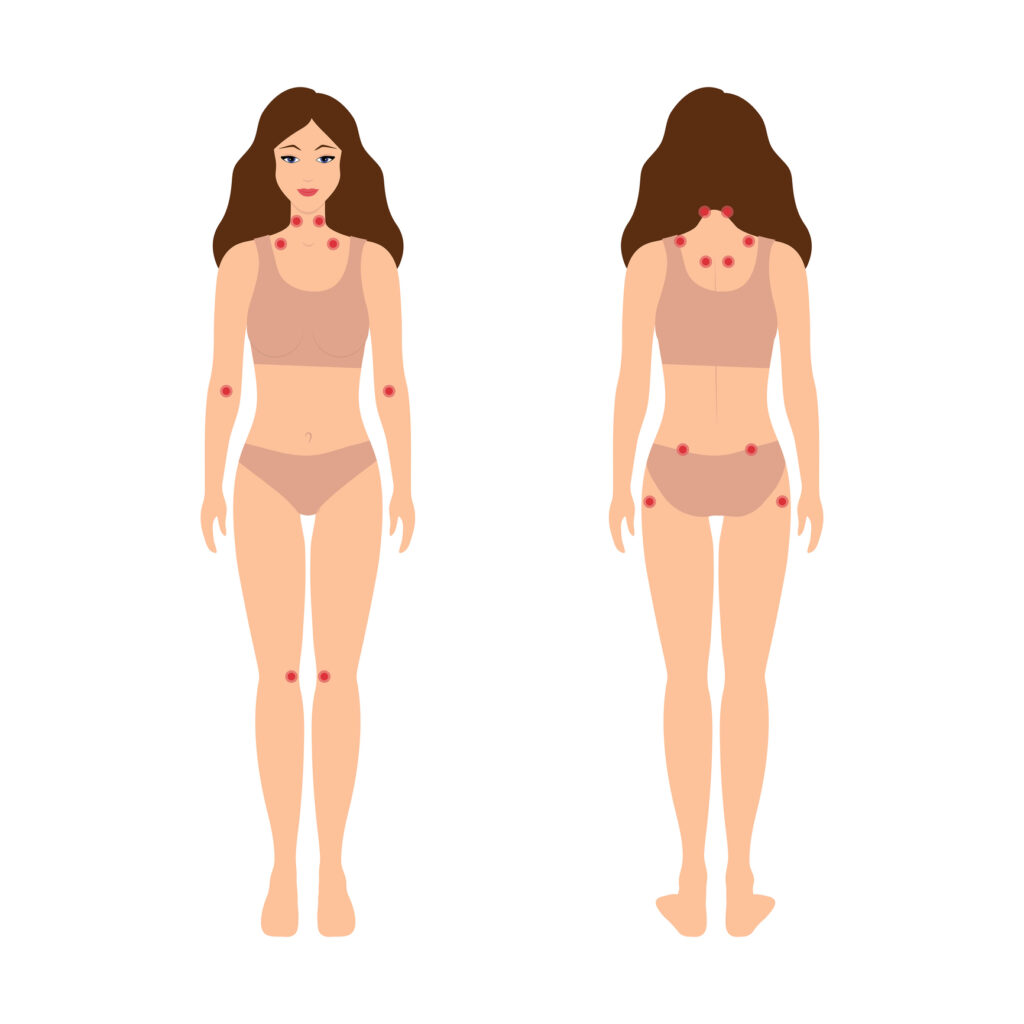 While not officially named fibromyalgia until 1976, the widespread pain and tenderness were first described in the early 1820s and initially called fibrositis. Doctors believed the condition was caused by inflammation within the body. Fibromyalgia was first recognized by the American Medical Association in 1987 and, in 1990, the American College of Rheumatology established diagnostic guidelines that included a list of 18 tender points on the body where patients must experience pain and tenderness.
While not officially named fibromyalgia until 1976, the widespread pain and tenderness were first described in the early 1820s and initially called fibrositis. Doctors believed the condition was caused by inflammation within the body. Fibromyalgia was first recognized by the American Medical Association in 1987 and, in 1990, the American College of Rheumatology established diagnostic guidelines that included a list of 18 tender points on the body where patients must experience pain and tenderness.
At this time, a fibromyalgia diagnosis required a positive pain response in at least 11 of these 18 tender points. This method, however, proved ineffective as those with fibromyalgia can experience varied pain areas from day to day. For example, one may have 15 pain points on one day, but only six on another.
In 2010, the American College of Rheumatology updated the diagnostic criteria. An additional update occurred in 2016 with criteria that not only addressed the widespread pain but also other common symptoms associated with fibromyalgia. We will explore the complete diagnostic criteria below.
Causes of Fibro
While the exact causes of fibro are not fully understood, many factors may contribute to its development.
- Abnormal pain processing – Individuals with fibromyalgia may have altered central nervous system processing of pain signals, leading to heightened sensitivity and amplification of pain.
- Genetic predisposition – Fibromyalgia tends to run in families, suggesting a genetic component in its development.
- Environmental triggers – Physical or emotional trauma, such as accidents, injuries, surgeries, or psychological stress, can act as triggers for the onset of symptoms.
- Hormonal imbalances – Hormonal fluctuations, particularly in serotonin, dopamine, and cortisol levels, may contribute to the development of fibromyalgia.
- Neurotransmitter abnormalities – Alterations in neurotransmitters involved in pain regulation, such as serotonin, norepinephrine, and substance P, may play a role.
- Infections – Certain infections, such as viral or bacterial infections, have been linked to the development of fibromyalgia.
- Autoimmune disorders – There is some overlap between fibro and autoimmune disorders, indicating a potential association.
It’s important to note that these factors likely interact and contribute to the development of fibromyalgia in different individuals, and further research is needed to fully understand the complexity of this condition.
Prevalence of Fibromyalgia
Fibromyalgia is a relatively common condition, with a global prevalence estimated to be around 2%-8% of the population. It is more commonly diagnosed in women than men, with a female-to-male ratio of approximately 3:1. Fibromyalgia can affect people of all ages, but it is most commonly diagnosed in middle-aged adults. The prevalence of fibromyalgia tends to increase with age, peaking in the 50s and 60s. However, it can also be diagnosed in children and adolescents.
It is important to note that fibromyalgia is often underdiagnosed or misdiagnosed, and many individuals may not seek medical attention or receive a proper diagnosis. Therefore, the actual prevalence of fibromyalgia may be higher than reported.
Fibromyalgia Risk Factors
While the exact cause of fibromyalgia is unknown, researchers believe that it may involve a combination of genetic, environmental, and psychological factors. Here are some potential risk factors that have been associated with the development of fibromyalgia:
- Gender – Fibromyalgia is more commonly diagnosed in women than in men. The reasons for this gender difference are not fully understood, but hormonal and genetic factors may play a role.
- Family history – There is evidence to suggest that fibromyalgia can run in families, indicating a possible genetic predisposition. Having a close relative, such as a parent or sibling, with fibro may increase your risk.
- Genetic factors – Certain genetic variations have been associated with an increased risk of developing fibromyalgia. However, more research is needed to understand the specific genes involved and their mechanisms.
- Physical trauma – Some individuals develop fibromyalgia symptoms after experiencing physical trauma, such as a car accident or injury. This suggests that physical trauma may trigger the onset of fibromyalgia in susceptible individuals.
- Psychological factors – Stress, anxiety, and depression have been linked to an increased risk of fibromyalgia. It is unclear whether these factors directly cause fibro or if they are secondary to living with chronic pain and other symptoms.
- Sleep disturbances – Disruptions in sleep patterns, such as insomnia or sleep apnea, have been associated with an increased risk of fibromyalgia. Sleep abnormalities may contribute to the development or worsening of fibromyalgia symptoms.
- Rheumatic diseases – Individuals with other rheumatic conditions, such as rheumatoid arthritis or lupus, may have a higher risk of developing fibromyalgia. The relationship between fibro and these conditions is complex and not fully understood.
- Viral infection – Research shows that prior viral infections, such as hepatitis B and C, Epstein-Barr virus (EBV), HIV, and Lyme disease may play a role in the development of fibromyalgia.
Common Symptoms
The hallmark symptom of fibromyalgia is widespread pain that affects multiple areas of the body. In terms of pain, patients may hear hyperalgesia (increased sensitivity to pain) and allodynia (pain response to a stimulus not normally associated with pain, such as a gentle touch). While pain is the most associated symptom of fibromyalgia, those with the condition experience many other symptoms that can include:
- Fatigue – People with fibromyalgia often experience persistent fatigue, even after getting enough sleep. This fatigue can be debilitating and may interfere with daily activities.
- Sleep disturbances – Many individuals with fibromyalgia have difficulties with sleep. They may have trouble falling asleep, staying asleep, or achieving restful sleep. This can contribute to the fatigue and overall sense of exhaustion they experience during daily life.
- Cognitive difficulties – Cognitive problems, commonly referred to as “fibro fog,” are common in fibromyalgia. This can include difficulties with memory, concentration, and attention, as well as mental confusion or difficulty finding the right words to complete a sentence or engage in conversation.
- Morning stiffness – Individuals with fibromyalgia often wake up in the morning feeling stiff and achy. This stiffness can make it challenging to get out of bed and start the day.
- Headaches – Chronic headaches, including tension headaches and migraines, are commonly reported by people with fibromyalgia.
- Irritable bowel syndrome (IBS) – Many individuals with fibro also experience gastrointestinal symptoms, such as abdominal pain, bloating, constipation, or diarrhea, which are characteristic of IBS.
- Sensitivity to sensory stimuli – People with fibromyalgia may be hypersensitive to various sensory stimuli, such as bright lights, loud noises, certain smells, or certain fabrics. This heightened sensitivity can trigger or worsen symptoms.
- Anxiety and depression – Fibro is often associated with psychological symptoms, including anxiety and depression. Living with chronic pain and other symptoms can significantly impact a person’s mental well-being.
Diagnosing Fibromyalgia
At this time, there are no specific laboratory or imaging tests that can show a definitive fibromyalgia diagnosis. Because fibro shares many of the same symptoms with other conditions, diagnosis often begins with ruling out any other potential conditions, such as osteoarthritis, rheumatoid arthritis, or lupus. After ruling out potential conditions, your clinician is likely to go over your medical history and perform a physical examination, looking at the areas you are experiencing pain.
The 1990 American College of Rheumatology classification criteria for a fibromyalgia diagnosis required 11 of 18 defined tender points. The tender points came with several limitations, such as “What pressure is enough to determine pain?” In 2010, the criteria changed, with additional modifications occurring in 2011 and 2016.
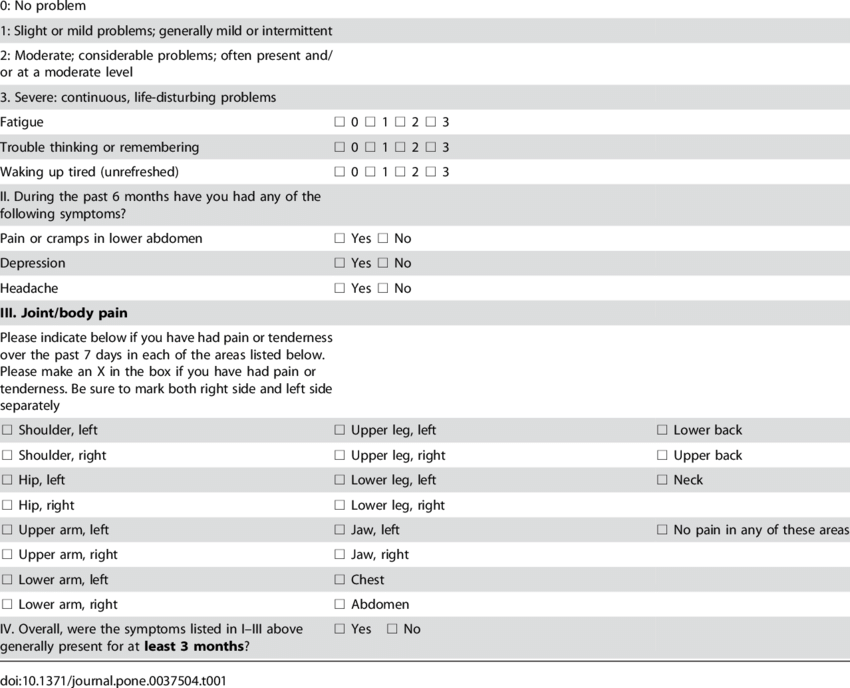
Current diagnostic criteria are based on three major components that are highlighted in the image below.
The first segment looks at the symptom severity scale for fatigue, cognitive function, and sleep. The second segment, or WPI (Widespread pain index), asks where the patient is experiencing pain, listing 19 locations on both sides of the body. The final segment asks if the symptoms have lasted over three months or longer.
Diagnostic criteria require a person to have either a WPI of at least 7 and an SS score of 5 or a WPI between 3-6 and an SS score of 9. These symptoms must also have been present for at least 3 months and no other underlying condition can explain the symptoms.
Treatment Options
Treatment for fibro can come from a clinician familiar with the condition, or you may receive a referral to a rheumatologist who specializes in fibro and other autoimmune conditions, such as rheumatoid arthritis and lupus. At this time, there is no cure for fibromyalgia and treatment strategies focus on managing symptoms and increasing quality of life. Potential treatments can include:
- Medications – These can include over-the-counter pain relievers, such as acetaminophen and ibuprofen, antidepressants like duloxetine and milnacipran to address pain and fatigue, and anti-seizure medications like gabapentin and pregabalin, often used to treat nerve pain.
- Therapeutic approach – Physical therapy and occupational therapy can help increase strength, flexibility, and stamina while also helping you to learn potential adjustments to daily activities that may help reduce pain symptoms.
Common Comorbidities
While fibro is enough on its own, it is often seen with additional comorbid conditions. Some of the common conditions seen with fibromyalgia include:
- Osteoarthritis
- Rheumatoid arthritis
- Lupus (systemic lupus erythematosus)
- Ankylosing spondylitis
- Dysautonomia, such as postural tachycardia syndrome (POTS)
- Migraine or other headaches
- Painful bladder syndrome
- Irritable bowel syndrome
- Anxiety and/or depression
- Temporomandibular joint (TMJ) disorders
- Myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS)
Fibromyalgia and Long COVID or ME/CFS
As we know, viral infections can often trigger additional health complications and the SARS-CoV-2 virus is no different. Researchers have linked COVID-19, Long COVID, and fibromyalgia in many different situations ranging from the idea that SARS-CoV-2 may act as a trigger for the development of fibro or as a trigger that worsens already existing fibromyalgia symptoms.
Whether you have an existing fibromyalgia diagnosis or believe your symptoms may fit the diagnostic criteria, the team of clinicians at RTHM are experienced in this and other similar conditions and comorbidities. When creating a treatment plan for Long COVID or ME/CFS, our team works with you to identify all potential underlying conditions and address them as needed to help improve your overall quality of life. Our goal is to quickly identify these underlying conditions and help you navigate a path that focuses on getting you better.

Get updates
Join our mailing list