Now live! RTHM Direct – simplified medication access for Long COVID, ME/CFS and related conditions. Check it out
The COVID-19 pandemic has brought with it a myriad of health challenges, some of which extend beyond the acute phase of the disease. One such issue is Long COVID, a condition characterized by lingering symptoms that persist for weeks, months, or years after the initial recovery. Among the many questions surrounding Long COVID, one that has gained significant attention is whether Long COVID can trigger Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS), a long-term illness that causes extreme fatigue.
Here we will explore the connection between Long COVID and ME/CFS and how continued research can help pave the way to effective treatment options.
Understanding ME/CFS and Long COVID
ME/CFS is a complex, chronic illness that affects multiple body systems, leading to symptoms like profound fatigue, unrefreshing sleep, cognitive impairment, and post-exertional malaise. The exact cause of ME/CFS remains unknown, but it’s often triggered by an infection.
Long COVID, on the other hand, refers to a range of symptoms that continue for more than four weeks after the onset of acute COVID-19. These symptoms can include fatigue, brain fog, breathlessness, and a host of others.
The Intersection of Long COVID and ME/CFS
In the wake of the COVID-19 pandemic, a significant number of patients are grappling with Long COVID, a condition characterized by lingering symptoms long after the acute phase of the virus. Recent research suggests that a substantial percentage of these Long COVID patients meet the diagnostic criteria for Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS).
ME/CFS and Post-Exertional Malaise Among Patients with Long COVID, published in Neurology International, looked at 465 patients with Long COVID. They concluded that among these patients, as many as 58 percent experienced symptoms associated with ME/CFS, such as profound fatigue, post-exertional malaise, unrefreshing sleep, and cognitive difficulties, and met the diagnostic criteria for ME/CFS. This intersection between Long COVID and ME/CFS has sparked a surge in research, aiming to unravel the complexities of these conditions and develop effective treatment strategies.
The Mechanism Behind the Connection
The mechanisms behind Long COVID and Myalgic Encephalomyelitis/Chronic Fatigue Syndrome (ME/CFS) are currently the subject of extensive scientific research. Both conditions are characterized by persistent fatigue, cognitive difficulties, and other debilitating symptoms.
Emerging evidence suggests that initial viral infection, such as SARS-CoV-2 in the case of Long COVID, may trigger a prolonged immune response, leading to chronic inflammation and a range of ongoing symptoms. This parallels theories about the onset of ME/CFS, where a viral trigger is often suspected, such as with the Epstein-Barr virus.
Additionally, some researchers propose that mitochondrial dysfunction might play a role in both conditions, leading to issues with energy production that could explain the profound fatigue experienced by patients.
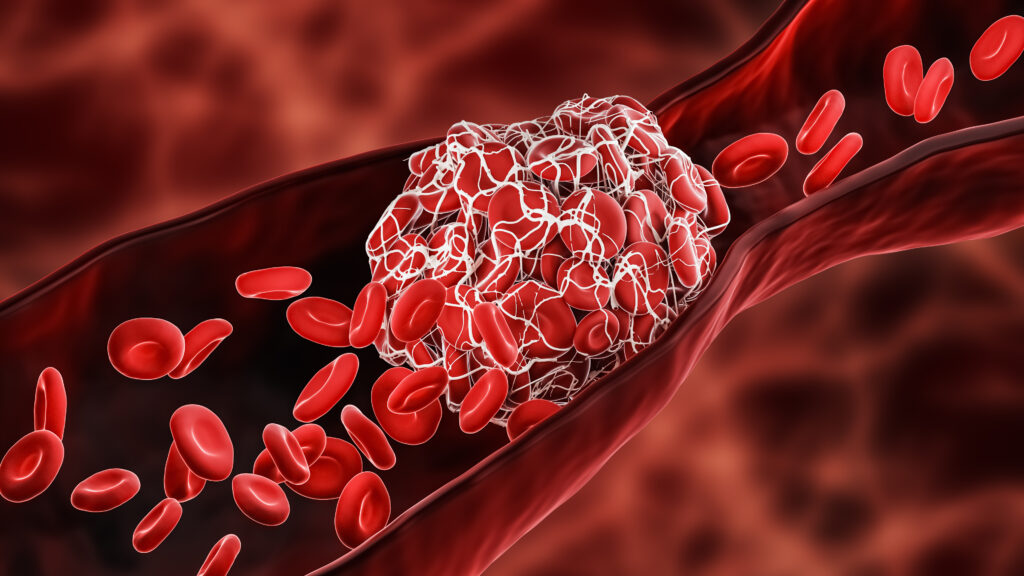
Other potential underlying causes researchers and clinicians are exploring for both Long COVID and ME/CFS are thrombotic endothelialitis, endothelial inflammation, hyperactivated platelets, and fibrinaloid microclots. These abnormalities can affect oxygen transportation throughout the body, affecting every organ and contributing to the symptoms patients with Long COVID and ME/CFS experience.
These insights are paving the way for a deeper understanding of these complex conditions and the development of targeted treatments.
Treating Both Long COVID and ME/CFS
While more research is needed to fully understand the connection between Long COVID and ME/CFS, current evidence suggests that Long COVID could indeed trigger ME/CFS in some individuals. This underscores the importance of ongoing research into both conditions, as well as the need for comprehensive care strategies to support those living with these chronic health challenges.
At RTHM, we believe that understanding the long-term effects of the SARS-CoV-2 virus, including the potential link to ME/CFS, is crucial. This knowledge will help us better manage Long COVID and shed light on the complex nature of ME/CFS, ultimately leading to improved treatments and outcomes for our patients. To learn more about Long COVID and ME/CFS care at RTHM, visit How It Works.

Get updates
Join our mailing list